Author: Munir Karjaghli, Clinical Applications Specialist, Hamilton Medical AG
Date of first publication: 15.11.2021

Takeaway messages
- Acute respiratory distress syndrome (ARDS) and acute lung injury (ALI) are frequently life‑threatening complications following major lung resection.
- One‑lung ventilation during and after thoracic surgery increases the risk of volutrauma, barotrauma, atelectrauma, and oxygen toxicity.
- Implementation of a protective ventilation protocol during OLV that includes permissive hypercapnia, reduced tidal volumes, increased positive end‑expiratory pressure, limited ventilator pressures, and recruitment maneuvers can reduce the risk of acute lung injury.
Causes of lung injury
Mechanical ventilation during one‑lung ventilation (OLV), also known as single‑lung ventilation, has three goals: (I) to aid in carbon dioxide elimination, (II) to maintain oxygenation, and (III) to reduce postoperative lung dysfunction. Numerous studies have been conducted to determine the most appropriate strategy for mechanical ventilation during OLV.
Many different factors can contribute to perioperative ALI. Lung injury results from mechanical stress caused by hyperinflation, hyperperfusion, and cyclic recruitment/de‑recruitment, together with proinflammatory or biochemical factors. In the case of thoracic surgery patients, a ‘multiple‑hit' theory suggests that a combination of surgery‑related factors, one‑lung ventilation, underlying diseases and co‑morbidities, prior therapy, and other unidentified events may result in greater susceptibility to ALI (
One‑lung ventilation during and after thoracic surgery increases the risk of volutrauma, barotrauma, atelectrauma, and oxygen toxicity, all of which are serious complications that cause ventilator‑induced lung injury (
What is protective one‑lung ventilation?
There is very little data that specifically supports a particular approach to management of OLV in terms of clinical outcomes. The definition of what is considered protective OLV is mainly influenced by expert opinion, evidence gathered from two‑lung ventilation in general surgical patients, and a small number of clinical trials. It is very difficult to pinpoint tidal volume, for example, as a single factor contributing to lung injury during OLV. No study to date has definitively demonstrated any specific advantage of low tidal volume (VT) ventilation during OLV in the absence of other ventilatory strategies, such as positive end‑expiratory pressure (PEEP) (
Driving pressure over tidal volume?
A retrospective study conducted after implementing a protective ventilation protocol during OLV for lung cancer surgery, which included reduced VT, increased PEEP, limited ventilator pressures, and recruitment maneuvers, found a lower risk of acute lung injury (
Practice guidelines for mechanical ventilation management during OLV
The Society for Translational Medicine presents recommendations based on the current evidence for one‑lung ventilation in their Clinical Practice Guidelines for mechanical ventilation management for patients undergoing lobectomy (
- Permissive/therapeutic hypercapnia, to maintain a partial pressure of carbon dioxide of 50 ‑70 mmHg may potentially be beneficial in patients undergoing single‑lung ventilation during pulmonary lobectomy operations.
- Protective ventilation with tidal volumes of 4‑6 ml/kg and a PEEP of 5‑8 cmH2O while trying to maintain a driving pressure < 15 cmH2O seems to be reasonable based on current evidence.
- Alveolar recruitment (open‑lung ventilation) may potentially be beneficial in patients undergoing lobectomy with one‑lung ventilation.
- Pressure‑controlled (CMV‑PC) or pressure‑controlled volume‑guaranteed ventilation (CMV‑vtPC) is recommended over volume‑controlled ventilation (CMV‑VC) and can be used in patients undergoing lung resection with single‑lung ventilation.
- Application of the lowest FiO2 necessary to maintain satisfactory arterial oxygen saturation is reasonable.
- Controlled mechanical ventilation with an I:E ratio of 1:1 or greater, is reasonable in patients undergoing one‑lung ventilation.
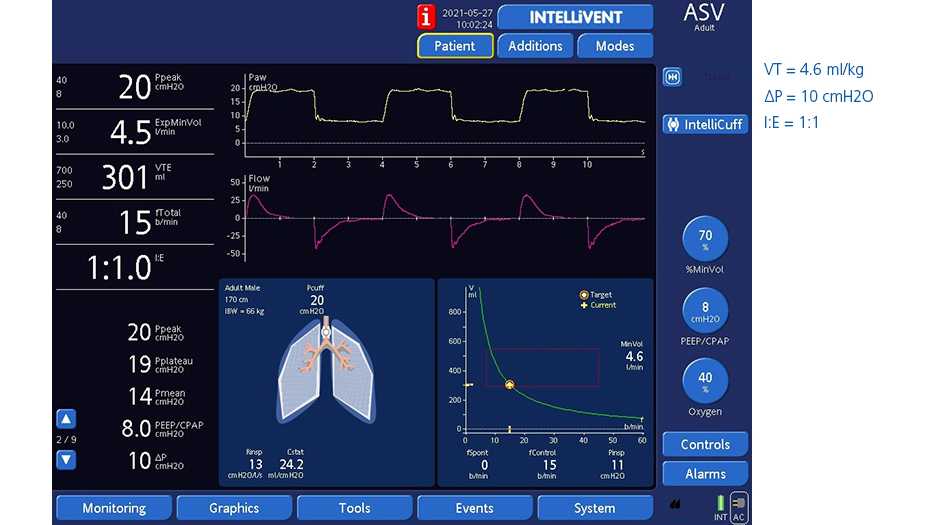
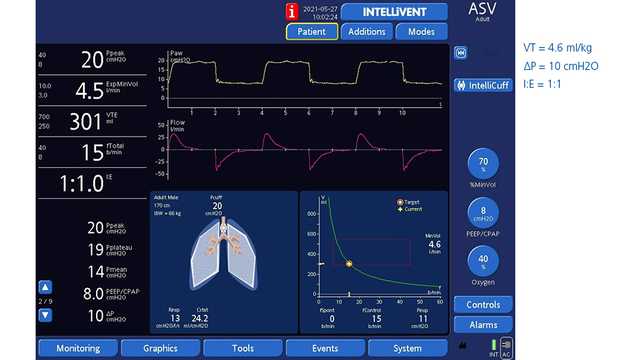
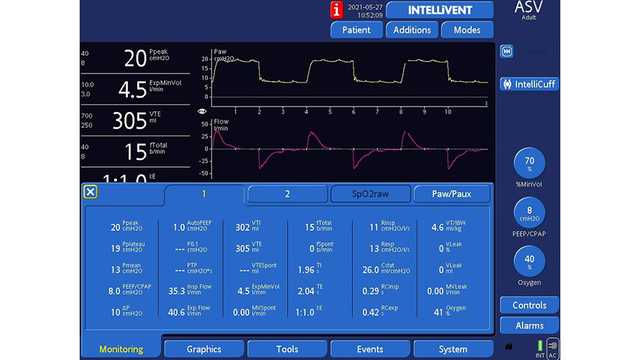
The Adapative Support Ventilation® (ASV®) mode on all Hamilton Medical ventilators automatically implements a lung‑protective strategy compliant with tidal volume recommendations and driving pressure in OLV. Additionally, the fully closed‑loop mode INTELLiVENT®‑ASV (
A study from Weiler et al. shows that ASV can ventilate patients safely, even under the highly variable conditions of OLV (
Figures 1 and 2 below show a 61‑year‑old male patient who underwent a right pneumonectomy being ventilated in ASV.
Full citations below: (
Footnotes
- A. Not available in the US and some other markets
References
- 1. Ruffini E, Parola A, Papalia E, et al. Frequency and mortality of acute lung injury and acute respiratory distress syndrome after pulmonary resection for bronchogenic carcinoma. Eur J Cardiothorac Surg. 2001;20(1):30‑37. doi:10.1016/s1010‑7940(01)00760‑6
- 2. Kutlu CA, Williams EA, Evans TW, Pastorino U, Goldstraw P. Acute lung injury and acute respiratory distress syndrome after pulmonary resection. Ann Thorac Surg. 2000;69(2):376‑380. doi:10.1016/s0003‑4975(99)01090‑5
- 3. Shapiro M, Swanson SJ, Wright CD, et al. Predictors of major morbidity and mortality after pneumonectomy utilizing the Society for Thoracic Surgeons General Thoracic Surgery Database. Ann Thorac Surg. 2010;90(3):927‑935. doi:10.1016/j.athoracsur.2010.05.041
- 4. Lytle FT, Brown DR. Appropriate ventilatory settings for thoracic surgery: intraoperative and postoperative. Semin Cardiothorac Vasc Anesth. 2008;12(2):97‑108. doi:10.1177/1089253208319869
- 5. Lohser J. Evidence‑based management of one‑lung ventilation. Anesthesiol Clin. 2008;26(2):241‑v. doi:10.1016/j.anclin.2008.01.011
- 6. Blank RS, Colquhoun DA, Durieux ME, et al. Management of One‑lung Ventilation: Impact of Tidal Volume on Complications after Thoracic Surgery. Anesthesiology. 2016;124(6):1286‑1295. doi:10.1097/ALN.0000000000001100
- 7. Slinger PD. Do Low Tidal Volumes Decrease Lung Injury During One‑Lung Ventilation?. J Cardiothorac Vasc Anesth. 2017;31(5):1774‑1775. doi:10.1053/j.jvca.2017.07.005
- 8. Levin MA, McCormick PJ, Lin HM, Hosseinian L, Fischer GW. Low intraoperative tidal volume ventilation with minimal PEEP is associated with increased mortality. Br J Anaesth. 2014;113(1):97‑108. doi:10.1093/bja/aeu054
- 9. Duggan M, Kavanagh BP. Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology. 2005;102(4):838‑854. doi:10.1097/00000542‑200504000‑00021
- 10. Licker M, Diaper J, Villiger Y, et al. Impact of intraoperative lung‑protective interventions in patients undergoing lung cancer surgery. Crit Care. 2009;13(2):R41. doi:10.1186/cc7762
- 11. Park M, Ahn HJ, Kim JA, et al. Driving Pressure during Thoracic Surgery: A Randomized Clinical Trial. Anesthesiology. 2019;130(3):385‑393. doi:10.1097/ALN.0000000000002600
- 12. Gao S, Zhang Z, Brunelli A, et al. The Society for Translational Medicine: clinical practice guidelines for mechanical ventilation management for patients undergoing lobectomy. J Thorac Dis. 2017;9(9):3246‑3254. doi:10.21037/jtd.2017.08.166
- 13. Weiler N, Eberle B, Heinrichs W. Adaptive lung ventilation (ALV) during anesthesia for pulmonary surgery: automatic response to transitions to and from one‑lung ventilation. J Clin Monit Comput. 1998;14(4):245‑252. doi:10.1023/a:1009974825237