
Author: Caroline Brown
Date of first publication: 16.10.2020
Last change: 06.10.2020
First published: 16.07.2020 ROX (values) at 12 hours after HFNC initiation (previously: intubation) were predictors of HFNC failure.The coronavirus pandemic has stretched many hospitals’ resources to the limit. Patients are requiring respiratory support on an unprecedented scale and a possible ‑ or in some cases very real ‑ shortage of ventilators is forcing institutions to weigh up the risks and benefits of alternative forms of therapy.

Takeaway messages
- Delivery of oxygen by high flow nasal cannula has a range of benefits including greater patient comfort, and improved oxygenation and ventilation.
- One of the major challenges is identifying those patients in which HFNC is likely to fail, as delayed intubation may result in worse outcomes.
- An index defined as the ratio of SpO2/FiO2 to the respiratory rate is an easy‑to‑use bedside tool that can help identify the need for mechanical ventilation in pneumonia patients with AHRF treated with HFNC.
Risks versus benefits for clinicians and patients
On the one hand, evidence on the use of oxygen delivered by high flow nasal cannula (HFNC) in patients with acute hypoxemic respiratory failure (AHRF) has demonstrated its superiority to standard oxygen therapy by facemask in many respects, including better tolerance, and improved oxygenation and work of breathing (
Application and benefits in a general setting
There are several mechanisms of action for HFNC that translate into a range of benefits, including greater patient comfort (
The ROX index
The ROX index is defined as the ratio of SpO2 (oxygen saturation as measured by pulse oximetry)/FiO2 (fraction of inspired oxygen) to the respiratory rate. SpO2/FiO2 has been shown to have a positive association with the success of HNFC, while RR has an inverse association. In their results published in 2016, Roca et al. concluded that the ROX index, which combined both parameters, could successfully be used to identify patients who were at low risk of HFNC failure and could therefore continue to receive HFNC after 12 hours (
Correlation between ROX index and increase in flow
Based on previous data from patients with AHRF treated with HFNC, which showed that the set flow rate has a significant effect on oxygenation and RR (
What is next?
On top of the limitations of previous studies, concerns have been expressed about the relationship between the SpO2/FiO2 ratio and the PaO2 (partial pressure of arterial oxygen)/FiO2 ratio that may not always be so linear (
Conclusion
The ROX index is an accurate, simple‑to‑use tool for any staff member at the bedside. As such, it could potentially be measured routinely in those patients undergoing HFNC. Further research will shed light on the feasibility and usefulness of using the ROX index in combination with traditional criteria for determining whether intubation is necessary.
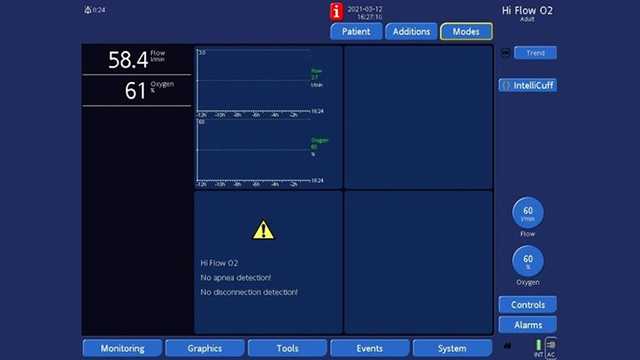
Ventilators from Hamilton Medical offer high flow oxygen therapy as a standard or optional feature, in addition to continuous SpO2 and SpO2/FiO2 measurement (
It is also available on our standalone high flow oxygen therapy device, the HAMILTON‑HF90 (

Free e‑book
The basics of high flow nasal cannula therapy
Our e‑book on high flow nasal cannula therapy gives you an overview of the working principles and clinical benefits, as well as practical information about choosing the right interface, adjusting the settings, and monitoring your patients.
Footnotes
- A. Some features are options. Not all features/products are available in all markets. Specifications are subject to change without notice.
References
- 1. Roca O, Riera J, Torres F, Masclans JR. High‑flow oxygen therapy in acute respiratory failure. Respir Care. 2010;55(4):408‑413.
- 2. Tiruvoipati R, Lewis D, Haji K, Botha J. High‑flow nasal oxygen vs high‑flow face mask: a randomized crossover trial in extubated patients. J Crit Care. 2010;25(3):463‑468. doi:10.1016/j.jcrc.2009.06.050
- 6. Ou X, Hua Y, Liu J, Gong C, Zhao W. Effect of high‑flow nasal cannula oxygen therapy in adults with acute hypoxemic respiratory failure: a meta‑analysis of randomized controlled trials. CMAJ. 2017;189(7):E260‑E267. doi:10.1503/cmaj.160570
- 7. Ferreyro BL, Angriman F, Munshi L, et al. Association of Noninvasive Oxygenation Strategies With All‑Cause Mortality in Adults With Acute Hypoxemic Respiratory Failure: A Systematic Review and Meta‑analysis. JAMA. 2020;324(1):57‑67. doi:10.1001/jama.2020.9524
- 8. Li J, Fink JB, Ehrmann S. High‑flow nasal cannula for COVID‑19 patients: low risk of bio‑aerosol dispersion. Eur Respir J. 2020;55(5):2000892. Published 2020 May 14. doi:10.1183/13993003.00892‑2020
- 8. Lyons C, Callaghan M. The use of high‑flow nasal oxygen in COVID‑19. Anaesthesia. 2020;75(7):843‑847. doi:10.1111/anae.15073
- 9. Rittayamai N, Tscheikuna J, Rujiwit P. High‑flow nasal cannula versus conventional oxygen therapy after endotracheal extubation: a randomized crossover physiologic study. Respir Care. 2014;59(4):485‑490. doi:10.4187/respcare.02397
- 10. Maggiore SM, Idone FA, Vaschetto R, et al. Nasal high‑flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med. 2014;190(3):282‑288. doi:10.1164/rccm.201402‑0364OC
- 11. Hasani A, Chapman TH, McCool D, Smith RE, Dilworth JP, Agnew JE. Domiciliary humidification improves lung mucociliary clearance in patients with bronchiectasis. Chron Respir Dis. 2008;5(2):81‑86. doi:10.1177/1479972307087190
- 12. Williams R, Rankin N, Smith T, Galler D, Seakins P. Relationship between the humidity and temperature of inspired gas and the function of the airway mucosa. Crit Care Med. 1996;24(11):1920‑1929. doi:10.1097/00003246‑199611000‑00025
- 13. Sztrymf B, Messika J, Mayot T, Lenglet H, Dreyfuss D, Ricard JD. Impact of high‑flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care. 2012;27(3):324.e9‑324.e3.24E13. doi:10.1016/j.jcrc.2011.07.075
- 14. Sztrymf B, Messika J, Bertrand F, et al. Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med. 2011;37(11):1780‑1786. doi:10.1007/s00134‑011‑2354‑6
- 15. Lenglet H, Sztrymf B, Leroy C, Brun P, Dreyfuss D, Ricard JD. Humidified high flow nasal oxygen during respiratory failure in the emergency department: feasibility and efficacy. Respir Care. 2012;57(11):1873‑1878. doi:10.4187/respcare.01575
- 16. Sim MA, Dean P, Kinsella J, Black R, Carter R, Hughes M. Performance of oxygen delivery devices when the breathing pattern of respiratory failure is simulated. Anaesthesia. 2008;63(9):938‑940. doi:10.1111/j.1365‑2044.2008.05536.x
- 17. Ritchie JE, Williams AB, Gerard C, Hockey H. Evaluation of a humidified nasal high‑flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. Anaesth Intensive Care. 2011;39(6):1103‑1110. doi:10.1177/0310057X1103900620
- 18. Wagstaff TA, Soni N. Performance of six types of oxygen delivery devices at varying respiratory rates. Anaesthesia. 2007;62(5):492‑503. doi:10.1111/j.1365‑2044.2007.05026.x
- 19. Groves N, Tobin A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care. 2007;20(4):126‑131. doi:10.1016/j.aucc.2007.08.001
- 20. Mauri T, Turrini C, Eronia N, et al. Physiologic Effects of High‑Flow Nasal Cannula in Acute Hypoxemic Respiratory Failure. Am J Respir Crit Care Med. 2017;195(9):1207‑1215. doi:10.1164/rccm.201605‑0916OC
- 21. Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF. Oxygen delivery through high‑flow nasal cannulae increase end‑expiratory lung volume and reduce respiratory rate in post‑cardiac surgical patients. Br J Anaesth. 2011;107(6):998‑1004. doi:10.1093/bja/aer265
- 22. Kang BJ, Koh Y, Lim CM, et al. Failure of high‑flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015;41(4):623‑632. doi:10.1007/s00134‑015‑3693‑5
- 23. Roca O, Messika J, Caralt B, et al. Predicting success of high‑flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J Crit Care. 2016;35:200‑205. doi:10.1016/j.jcrc.2016.05.022
- 24. Roca O, Caralt B, Messika J, et al. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High‑Flow Therapy. Am J Respir Crit Care Med. 2019;199(11):1368‑1376. doi:10.1164/rccm.201803‑0589OC
- 25. Mauri T, Alban L, Turrini C, et al. Optimum support by high‑flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43(10):1453‑1463. doi:10.1007/s00134‑017‑4890‑1
- 26. Mauri T, Carlesso E, Spinelli E, et al. Increasing support by nasal high flow acutely modifies the ROX index in hypoxemic patients: A physiologic study. J Crit Care. 2019;53:183‑185. doi:10.1016/j.jcrc.2019.06.020
- 27. Brown SM, Grissom CK, Moss M, et al. Nonlinear Imputation of Pao2/Fio2 From Spo2/Fio2 Among Patients With Acute Respiratory Distress Syndrome. Chest. 2016;150(2):307‑313. doi:10.1016/j.chest.2016.01.003
- 28. Brown SM, Grissom CK, Moss M, et al. Nonlinear Imputation of Pao2/Fio2 From Spo2/Fio2 Among Patients With Acute Respiratory Distress Syndrome. Chest. 2016;150(2):307‑313. doi:10.1016/j.chest.2016.01.003
- 4,. Rochwerg B, Granton D, Wang DX, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta‑analysis. Intensive Care Med. 2019;45(5):563‑572. doi:10.1007/s00134‑019‑05590‑5
Related articles. Get a deeper look

The complete guide to high flow nasal cannula therapy (HFNC)
Everything healthcare professionals need to know to get started with high flow nasal cannula therapy: the flow rate, FiO2 settings, when to use HFNC, selecting the interface, and much more.
How to use high flow therapy in COVID‑19 acute hypoxemic respiratory failure
High flow therapy (HFT) has been used widely during the COVID‑19 pandemic. Published clinical experience is based mainly on retrospective studies and describes the main settings and the failure rate.



