
Author: Caroline Brown, Giorgio Iotti
Date of first publication: 08.07.2022
Asynchrony between patient and ventilator is a common occurrence in mechanically ventilated patients (1, 2).

Takeaway messages
- The concept of analyzing pressure and flow waveforms to detect respiratory efforts was first described decades ago but subsequent evidence on the reliability of this approach is not clear.
- In a recent study, investigators evaluated a systematic method of waveform analysis for assessing patient activity and patient‑ventilator interaction at the bedside, using a Pes curve as a reference.
- The waveform method enabled clinicians to detect an extremely high percentage of spontaneous efforts and was shown to be a highly reproducible and reliable means of identifying even minor asynchronies.
An important part of treatment
This mismatch between the inspiratory and expiratory times of patient and ventilator may take various forms, such as early or late cycling, auto‑triggering, double triggering, or ineffective efforts, and has been shown to impact on patient outcomes (
The concept of analyzing airway pressure and flow waveforms to detect respiratory efforts and their timing was first described almost three decades ago (
Applying the waveform method
A key element of this trial was the use of a systematic method to analyze the airway pressure and flow waveforms, which comprised five general physiological principles and a set of specific rules defined beforehand (“the waveform method”). All patients were ventilated in pressure‑support mode with an esophageal catheter in place. The method was applied to the airway pressure and flow waveforms that were obtained using a proximal sensor, and esophageal pressure (Pes) was used as a reference. For each patient, three researchers from a team of four (three senior physicians and one resident) analyzed the flow and pressure waveforms only, while another researcher analyzed flow and pressure waveforms as well as the Pes tracing. The breaths were classified as either “normally” assisted, auto‑triggered, double triggered, or ineffective efforts. In the case of normally assisted breaths, minor asynchronies (trigger delay, early cycling, and late cycling) were also evaluated.
Endpoints and results
The primary endpoint was the percentage of spontaneous efforts detected using the waveform method. Amongst the secondary endpoints were the agreement between the waveform and reference methods in detecting major and minor asynchronies, as well as the inter‑rater agreement for the waveform method.
A total of 4,426 breaths were recorded. Using the reference Pes measurements, 77.8% of these were identified as breaths correctly detected by the ventilator, 22.1% as ineffective efforts, and 0.1% as auto‑triggered breaths. The waveform method was able to detect 99.5% of the spontaneous efforts and all but one of the auto‑triggered breaths. Similarly, agreement between the reference and waveform methods for identifying breaths as assisted, auto‑triggered, double triggered or ineffective was very high. The Asynchrony Index ‑ calculated as the sum of auto‑triggered, ineffective, and double‑triggered breaths divided by the total number of breaths ‑ was 5.9% and did not differ when assessed using the waveform method versus esophageal pressure. The total Asynchrony Time ‑ calculated as the time during which the ventilator and the patient were not synchronous divided by the total recording time ‑ was 22.4%, with minor asynchronies accounting for 92.1% of it. Agreement amongst the different operators for classifying the breaths was also very high.
In more than 90% of the cases, the waveform method enabled the researchers to identify the start and the end of the respiratory efforts with sufficient precision that correct identification of the “minor” asynchronies ‑ trigger delay, early cycling, and late cycling ‑ was also possible.
What do these results tell us?
This study presents some important findings. The investigators show that the waveform method enables clinicians to detect an extremely high percentage of spontaneous efforts and precisely assess the timing the patient’s activity. Even for minor asynchronies, the waveform method is both highly reliable and reproducible. The importance of this is underlined by a further finding of the study, namely that the majority of the asynchrony time in PSV was related to minor asynchronies.
Not only do these results demonstrate the reproducibility of the waveform method (high inter‑operator agreement); they also indicate that training in waveform analysis according to a predefined, systematic method plays a pivotal role. Evidence has shown that clinical experience with treating mechanically ventilated patients does not necessarily equate with competence in recognizing asynchronies, which is overall quite low in ICU physicians (
The authors conclude that proximal waveforms of airway pressure and airflow include sufficient information for accurately assessing patient activity and patient‑ventilator interaction, assuming that an appropriate systematic method of analysis such as the “the waveform method” is adopted.
Continuous analysis with IntelliSync+
The IntelliSync®+ technology integrated into Hamilton Medical ventilators (
Full citations below: (

Learn to spot common asynchronies! Free reference card
Our asynchrony reference card gives you an overview of the most common asynchrony types, their causes, and how to detect them.
Footnotes
- A. IntelliSync+ is available as an optional feature on the HAMILTON‑C6 and HAMILTON‑G5 mechanical ventilators, and is standard on the HAMILTON‑S1.
References
- 1. Chao DC, Scheinhorn DJ, Stearn‑Hassenpflug M. Patient‑ventilator trigger asynchrony in prolonged mechanical ventilation. Chest. 1997;112(6):1592‑1599. doi:10.1378/chest.112.6.1592
- 2. Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient‑ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32(10):1515‑1522. doi:10.1007/s00134‑006‑0301‑8
- 3. de Wit M, Miller KB, Green DA, Ostman HE, Gennings C, Epstein SK. Ineffective triggering predicts increased duration of mechanical ventilation. Crit Care Med. 2009;37(10):2740‑2745. doi:10.1097/ccm.0b013e3181a98a05
- 4. Blanch L, Villagra A, Sales B, et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 2015;41(4):633‑641. doi:10.1007/s00134‑015‑3692‑6
- 5. Fabry B, Guttmann J, Eberhard L, Bauer T, Haberthür C, Wolff G. An analysis of desynchronization between the spontaneously breathing patient and ventilator during inspiratory pressure support. Chest. 1995;107(5):1387‑1394. doi:10.1378/chest.107.5.1387
- 6. Giannouli E, Webster K, Roberts D, Younes M. Response of ventilator‑dependent patients to different levels of pressure support and proportional assist. Am J Respir Crit Care Med. 1999;159(6):1716‑1725. doi:10.1164/ajrccm.159.6.9704025
- 7. Colombo D, Cammarota G, Alemani M, et al. Efficacy of ventilator waveforms observation in detecting patient‑ventilator asynchrony. Crit Care Med. 2011;39(11):2452‑2457. doi:10.1097/CCM.0b013e318225753c
- 8. Mojoli F, Pozzi M, Orlando A, et al. Timing of inspiratory muscle activity detected from airway pressure and flow during pressure support ventilation: the waveform method. Crit Care. 2022;26(1):32. Published 2022 Jan 30. doi:10.1186/s13054‑022‑03895‑4
- 9. Ramirez II, Arellano DH, Adasme RS, et al. Ability of ICU Health‑Care Professionals to Identify Patient‑Ventilator Asynchrony Using Waveform Analysis. Respir Care. 2017;62(2):144‑149. doi:10.4187/respcare.04750
Related articles. Get a deeper look
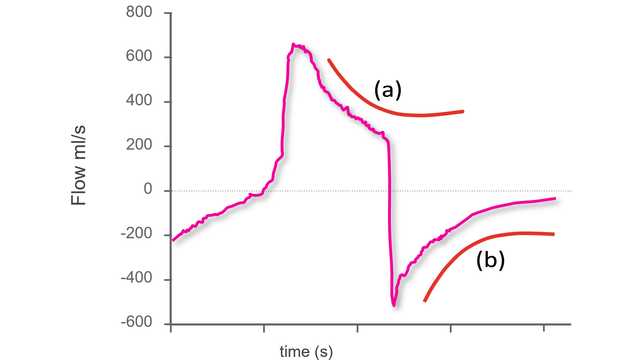
Using waveforms to indentify asynchronies ‑ Step 1
The first step to identifying asynchronies using standard ventilator waveforms is knowing what a synchronous breath looks like during pressure‑support ventilation.
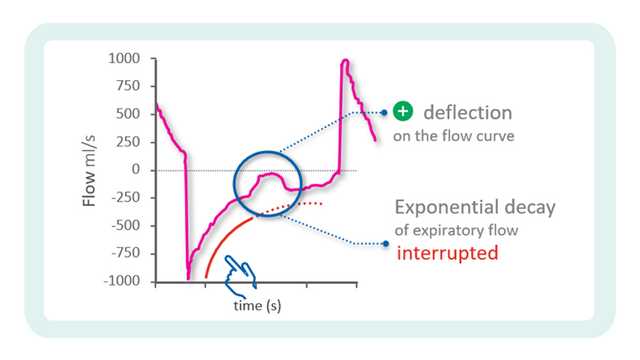
Using waveforms to identify asynchronies ‑ Step 2
In the previous issue, our Bedside tip covered the starting point for identifying asynchronies using ventilator waveforms.


