Author: Dr. med. Jean‑Michel Arnal, Senior Intensivist, Hopital Sainte Musse, Toulon, France
Date of first publication: 17.06.2020
Last change: 17.06.2020
First published 25.04.2018: Resistance cm2/l/s changed to cm2/(l/s)
Take‑away messages
Take‑away messages
- Monitoring respiratory mechanics helps to assess and diagnose the lung condition and impairment, and adjust the ventilator settings.
- The two main products of respiratory mechanics are compliance and resistance.
- The time constant describes the speed of the change in volume after a step change in pressure and is the product of resistance and compliance, measured at inspiration or expiration.
- The expiratory time constant is very useful for assessing the overall respiratory mechanics and the changes in them.
- A short expiratory time constant indicates a decrease in compliance, while a long one indicates increased resistance.
Measurement of respiratory mechanics
The main properties of respiratory mechanics are compliance and resistance. Other properties, such as inertia and viscoelasticity, do not play a significant role in conventional mechanical ventilation and can therefore be discounted. Respiratory mechanics are usually measured using airway pressure and flow; therefore, the assessment of the respiratory system’s properties includes the endotracheal tube. However, more precise measurements may be obtained in particular cases by using tracheal pressure at the carina, which enables us to separate the endotracheal tube and airway resistance. Esophageal pressure allows us to partition the chest wall and lung compliance. Static measurement of respiratory mechanics relies on end‑inspiratory and end‑expiratory occlusions, whereas dynamic measurement uses the least squares fitting method to assess compliance and resistance continuously during mechanical ventilation with no occlusion required (
Compliance
Compliance (C) describes the elastic property of the respiratory system including the lung and the chest wall. Static compliance (CSTAT) is the ratio between a change in volume (VT) and the corresponding change in transmural pressure (ΔP). The change in transmural pressure can be calculated as the difference between plateau pressure (PPLAT) and total PEEP (PEEPTOT) measured by an end‑inspiratory and end‑expiratory occlusion, respectively.
CSTAT = VT/ΔP = VT/ (PPLAT ‑ PEEPTOT)
The dimension of compliance is usually ml/cmH2O. Elastance (E) is the reciprocal of static compliance.
E= ΔP/ VT
Static compliance can be measured dynamically and continuously using the least squares fitting method (LSF) (
In patients with a normal lung undergoing mechanical ventilation, CSTAT is 50‑60 ml/cmH2O (
An increase in compliance occurs in the case of lung emphysema.
Resistance
Resistance (R) describes the opposition to a gas flow entering the respiratory system during inspiration, which is caused by frictional forces. Resistance is calculated as the ratio between the pressure driving a given flow and the resulting flow rate (V̇).
R = ΔP / V̇
The dimension of resistance is usually cmH2O/(l/s).
The resistance of the respiratory system is primarily made up of the resistance of the airways and the endotracheal tube, because the resistance of the lung tissue is low.
Resistance can only be calculated in volume‑control mode with a constant flow rate during inspiration.
RINSP = (PPEAK ‑ PPLAT)/ V̇INSP
However, resistance is usually measured continuously using the least squares fitting method, which allows for differentiation between inspiratory and expiratory resistance. It is normal that the expiratory resistance is higher than the inspiratory resistance due to the shape of the airway tree, but a large discrepancy between inspiratory and expiratory resistance may suggest an expiratory flow limitation.
In mechanically ventilated patients with a normal lung and an artificial airway, inspiratory resistance (RINSP) is 10‑15 cmH2O/(l/s) (
Time constant
The time constant (RC) describes the speed of the change in volume after a step change in pressure and can be measured at both inspiration and expiration. The dimension is time expressed in seconds.
Due to the fact that a step change in pressure is associated with a change of volume according to an exponential curve, the exponential function indicates that it takes 1, 2, and 3 time constants to change the volume by 63%, 86%, and 95% of the total volume change.
Assuming a monocompartmental lung model, RC is the product of compliance and resistance measured at inspiration or expiration.
CINSP= CSTAT x RINSP
RCEXP = CSTAT x REXP
As obstructive‑disease patients have bicompartmental expiration mainly due to an expiratory flow limitation, measuring RCEXP at 75% of the expired tidal volume will provide a more accurate result for the time constant of the slow compartment (
Its dependence on C and R means that RCEXP is very useful for assessing the overall respiratory mechanics and the changes in them. The measurement is accurate in both passive and spontaneously breathing patients, assuming there is passive expiration. It can also be measured during noninvasive ventilation, provided there are no unintentional leaks.
Typical values for RCEXP in mechanically ventilated patients with a normal lung are 0.5‑0.7 s. A short time constant indicates a decrease in compliance, while a long time constant occurs in the case of increased resistance. A mixed condition with a decrease in compliance and an increase in resistance can result in a pseudo‑normal RCEXP.
Table 1: Typical values for respiratory mechanics in adult ICU patients intubated and passively mechanically ventilated
| Normal lungs | ARDS | COPD | |
| Compliance (ml/cmH2O) | 50‑60 | 35‑45 | 50‑70 |
| Resistance (cmH2O.s/l) | 10‑15 | 10‑15 | 15‑30 |
| Expiratory time constant (s) | 0.5‑0.7 | 0.4‑0.6 | 0.7‑2.1 |
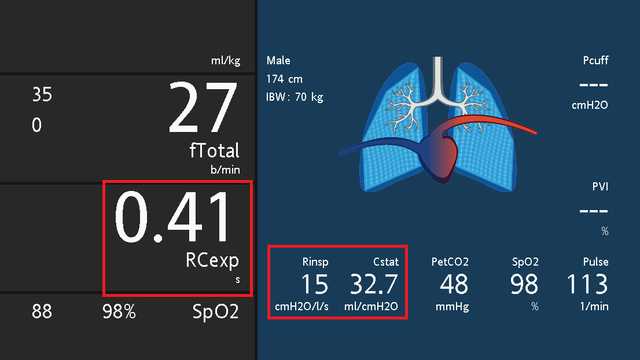
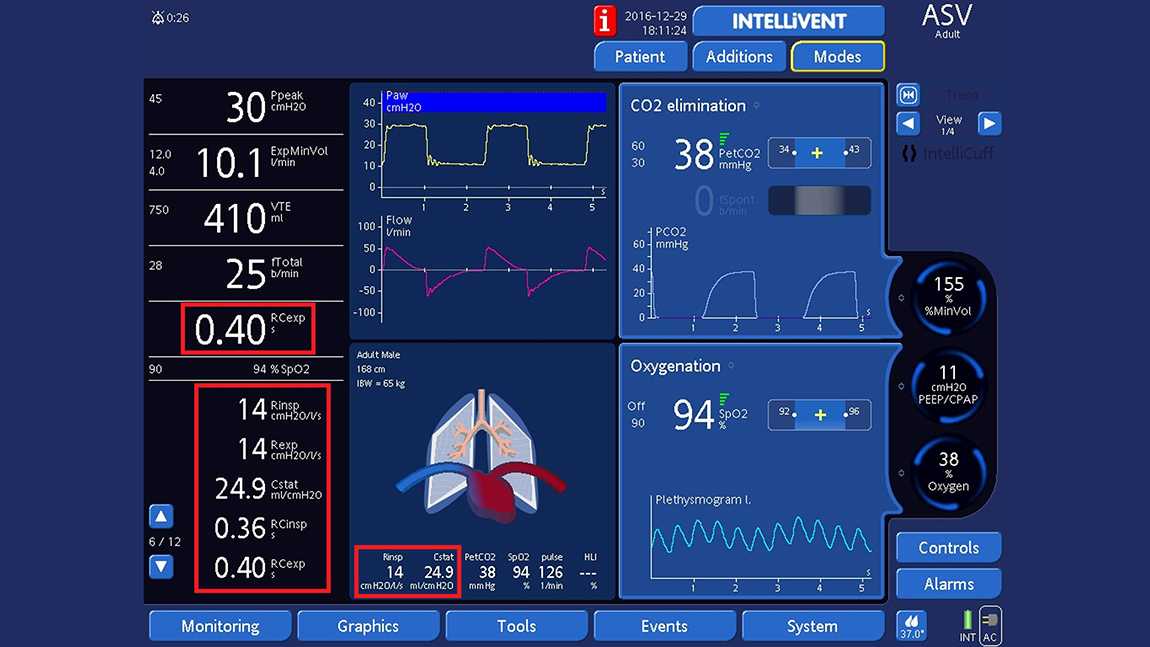
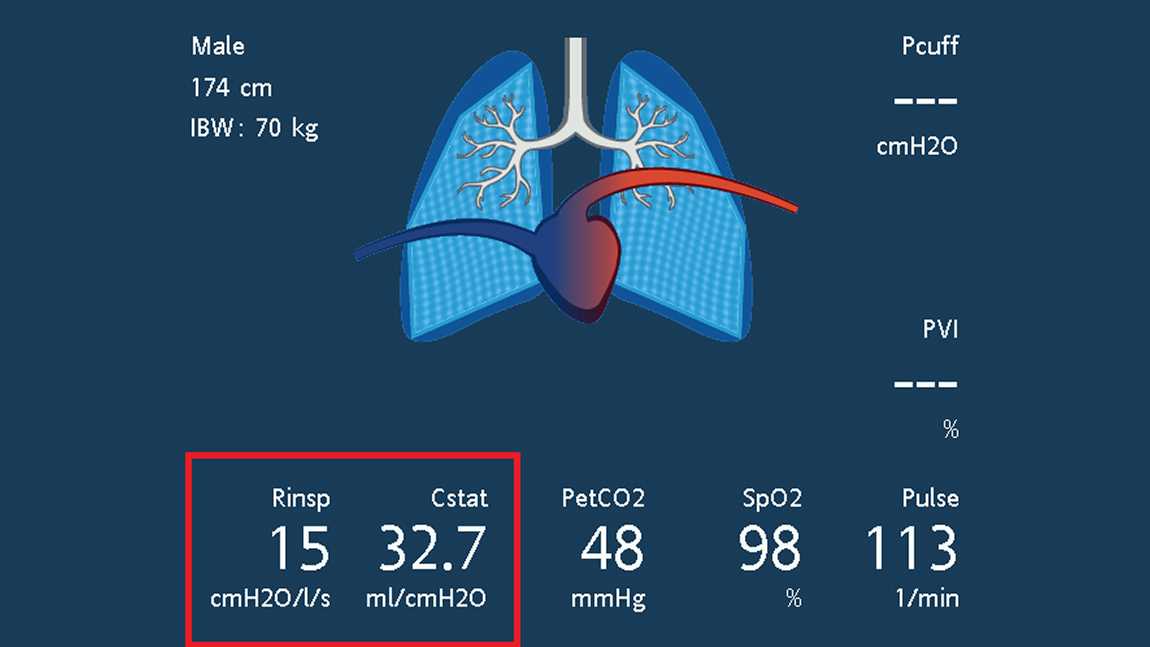
Expiratory time constant on Hamilton Medical ventilators
Hamilton Medical ventilators measure the RCEXP breath‑by‑breath at 75% of the expiratory volume and use the least squares fitting method to continuously calculate compliance, as well as inspiratory and expiratory resistance. Results are shown on the monitoring panel and the Dynamic Lung (see Figs 1 and 2), and trends for all variables of respiratory mechanics can be displayed. In addition, clinicians can make their own measurements of CSTAT and REXP using the occlusion method.


Footnotes
References
- 1. Brunner JX, Langenstein H, Wolff G. A simple method for estimating compliance. Crit Care Med. 1985;13(8):675‑678. doi:10.1097/00003246‑198508000‑00014
- 2. Iotti GA, Braschi A, Brunner JX, et al. Respiratory mechanics by least squares fitting in mechanically ventilated patients: applications during paralysis and during pressure support ventilation. Intensive Care Med. 1995;21(5):406‑413. doi:10.1007/BF01707409
- 3. Arnal JM, Garnero A, Saoli M, Chatburn RL. Parameters for Simulation of Adult Subjects During Mechanical Ventilation. Respir Care. 2018;63(2):158‑168. doi:10.4187/respcare.05775
- 4. Gerbeaux P, Gainnier M, Arnal JM, Papazian L, Jean P, Sainty JM. Effects of helium‑oxygen mixtures on endotracheal tubes: an in vitro study. J Biomech. 2005;38(1):33‑37. doi:10.1016/j.jbiomech.2004.03.019
- 5. Brunner JX, Laubscher TP, Banner MJ, Iotti G, Braschi A. Simple method to measure total expiratory time constant based on the passive expiratory flow‑volume curve. Crit Care Med. 1995;23(6):1117‑1122. doi:10.1097/00003246‑199506000‑00019
- 6. Lourens MS, van den Berg B, Aerts JG, Verbraak AF, Hoogsteden HC, Bogaard JM. Expiratory time constants in mechanically ventilated patients with and without COPD. Intensive Care Med. 2000;26(11):1612‑1618. doi:10.1007/s001340000632