Author: Dr. med. Jean‑Michel Arnal, Senior Intensivist, Hopital Sainte Musse, Toulon, France
Date of first publication: 25.04.2018
Product of compliance and resistance
RCexp is reliable in both passive and spontaneously breathing patients, assuming expiration is passive. It may also be used during NIV, provided there are no unintentional leaks.
As RCexp is the product of compliance and resistance, this single variable can provide us with an assessment of the overall respiratory mechanics. It is very useful for diagnosing the lung condition and its severity, optimizing the ventilator settings, monitoring prone positioning, and understanding certain respiratory events.
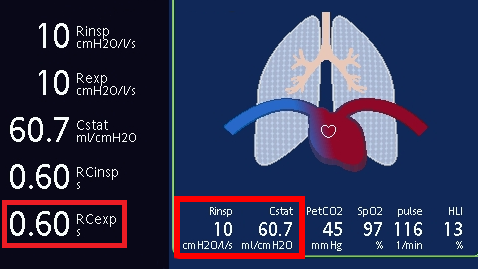
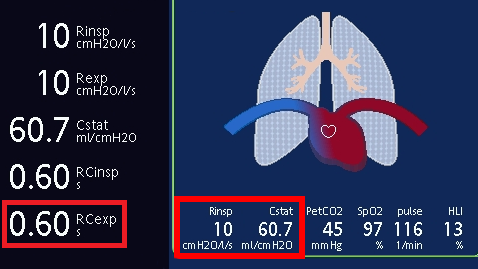
Expiratory time constant in a normal lung
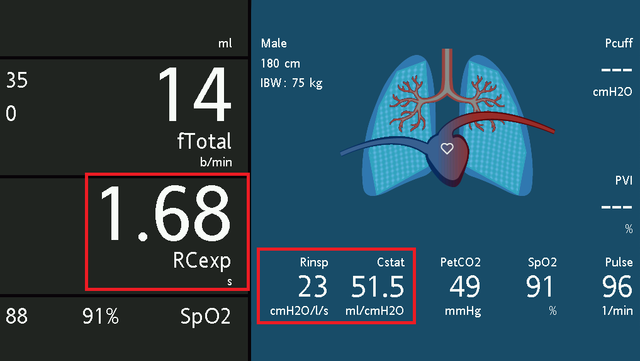
In a mechanically ventilated patient with a normal lung, RCexp is normally between 0.5 and 0.7 s (see Figure 1). However, it is important to check that compliance and resistance values are also within a normal range, because a mixed lung condition combining decreased compliance and increased resistance may result in a pseudo‑normal RCexp.
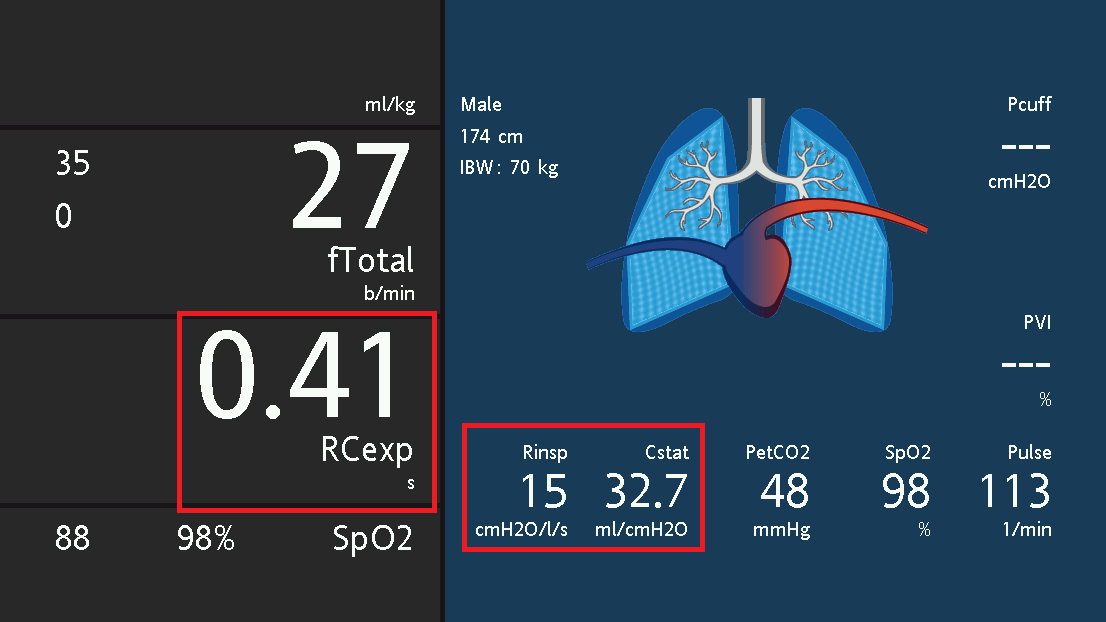
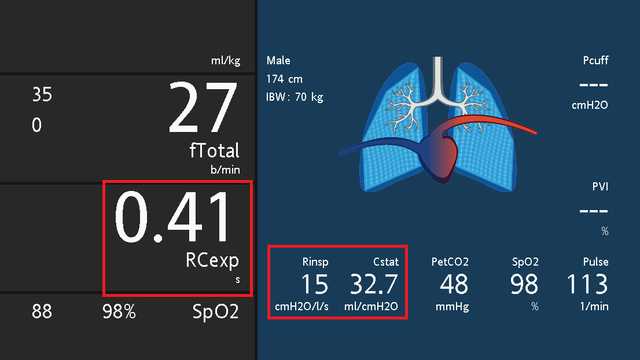
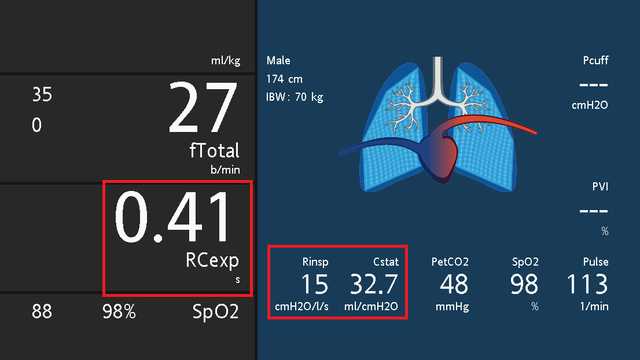
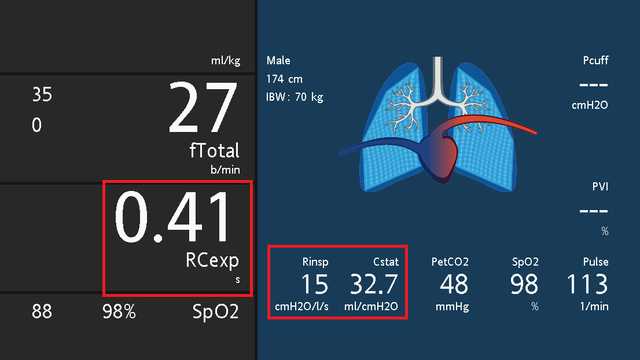
A short expiratory time constant
An expiratory time constant shorter than 0.5 s indicates a decrease in compliance, either due to the lung or the chest wall (see Figure 2). In ARDS patients, RCexp is typically in the range of 0.4 to 0.6 s. It is shorter in patients with more severe ARDS, indicating low compliance and a small volume of aerated lung. In patients with lung fibrosis or chest‑wall stiffness such as kyphoscoliosis, RCexp is usually very short and ranges from 0.15 to 0.25 s.
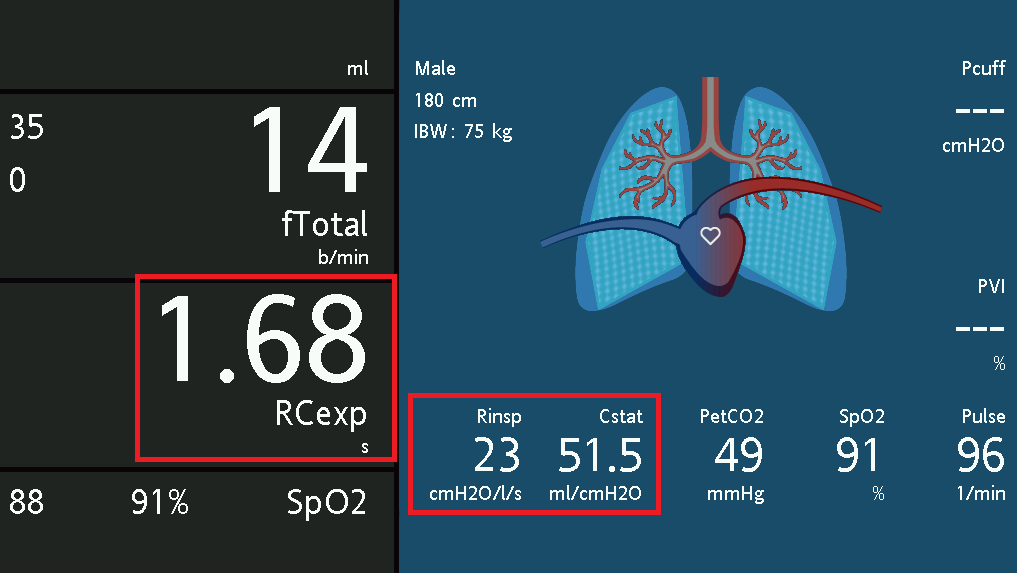
A long expiratory time constant
An expiratory time constant of longer than 0.7 s indicates increased resistance, which may be associated with increased compliance in the case of COPD patients with lung emphysema (see Figure 3). A long RCexp is typical in COPD and asthmatic patients. In patients with severe bronchospasm, RCexp can be as long as 3 s. If the patient is not COPD or asthmatic, a long RCexp may indicate incorrect positioning or kinking of the endotracheal tube.
RCexp for optimizing ventilator settings
Patients with a short RCexp are at risk of ventilator‑induced lung injuries and should be closely monitored for tidal volume, driving pressure, and plateau pressure. In contrast, patients with a long RCexp are at risk of dynamic hyperinflation, so intrinsic PEEP should be measured regularly.
In pressure‑support and ASV® modes, expiratory trigger sensitivity (ETS) is an important setting for optimizing patient‑ventilator synchronization. ETS represents the percentage of the maximum inspiratory flow at which the mechanical breath ends. A high percentage results in a short mechanical breath and vice versa. This setting can be optimized according to the respiratory mechanics.
Adjusting ETS based on RCexp
As an initial approach, ETS may be adjusted based on RCexp as follows:
| RCexp | ETS |
|---|---|
| Normal | 25%‑40% |
| Short | 5%‑25% |
| Long | 40%‑70% |
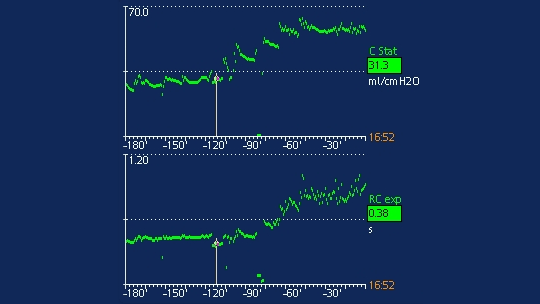
RCexp for monitoring prone positioning
The effect of prone positioning on respiratory mechanics can be assessed using the trend of RCexp and compliance. If prone positioning is associated with lung recruitment, it is indicated by an increase in compliance and RCexp. If RCexp increases with no change to compliance, the clinician should check for incorrect positioning or kinking of the endotracheal tube.
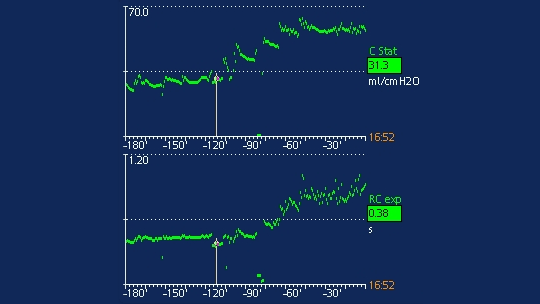
The image below displays an example of respiratory mechanics trends in the supine and prone position. The cursor indicates the start of the prone‑position session. After prone positioning, RCexp and compliance both increase, indicating lung recruitment (Figure 4).
RCexp for understanding respiratory events
A sudden event leading to desaturation and/or an increase in airway pressure needs a rapid diagnosis. Looking at trends for RCexp will help us to understand whether the event is related to a rapid change in respiratory mechanics. An increase in RCexp indicates one of the following: an endotracheal tube obstruction or malpositioning, a patient biting the endotracheal tube, an excess of secretions, or a bronchospasm. Conversely, a decrease in RCexp indicates a pneumothorax, pleural effusion, or atelectasis. Sudden desaturation without a change in RCexp indicates a drop in cardiac output or a severe pulmonary embolism.
Full citations below: (