Author: David Grooms
Date of first publication: 08.07.2019

Takeaway messages
- Mismatches between the patient and ventilator, also known as dyssynchronies, are a frequent occurrence in mechanically ventilated patients.
- One of the most prevalent forms is double triggering, which is usually due to improper matching of mechanical breath I‑times to neural I‑times and of particular concern in ARDS patients as it may lead to excessive tidal volume delivery.
- Diagnosing double triggering and differentiating between the three different types can represent a considerable challenge, and requires close observation and analysis of the ventilator’s scalar waveforms.
- New technology may assist clinicians in avoiding double triggering by automatically adjusting the inspiratory time in accordance with the patient’s needs.
What is double triggering?
The frequency of dyssynchronies has been studied and they are estimated to occur at least one time in no less than 50% of patients who receive mechanical ventilation (MV) for more than 24 hours. The two most common dyssynchronies are ineffective (missed) triggering and double triggering (DT) (
Diagnosis and resolution
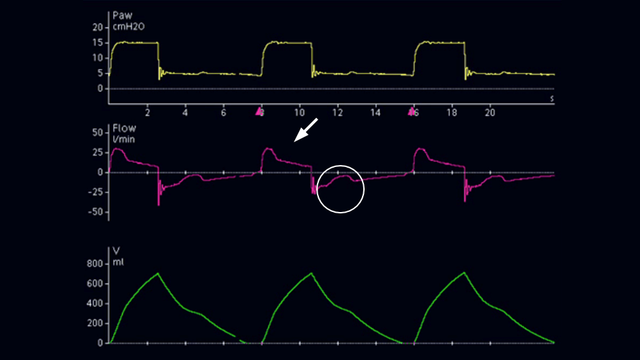
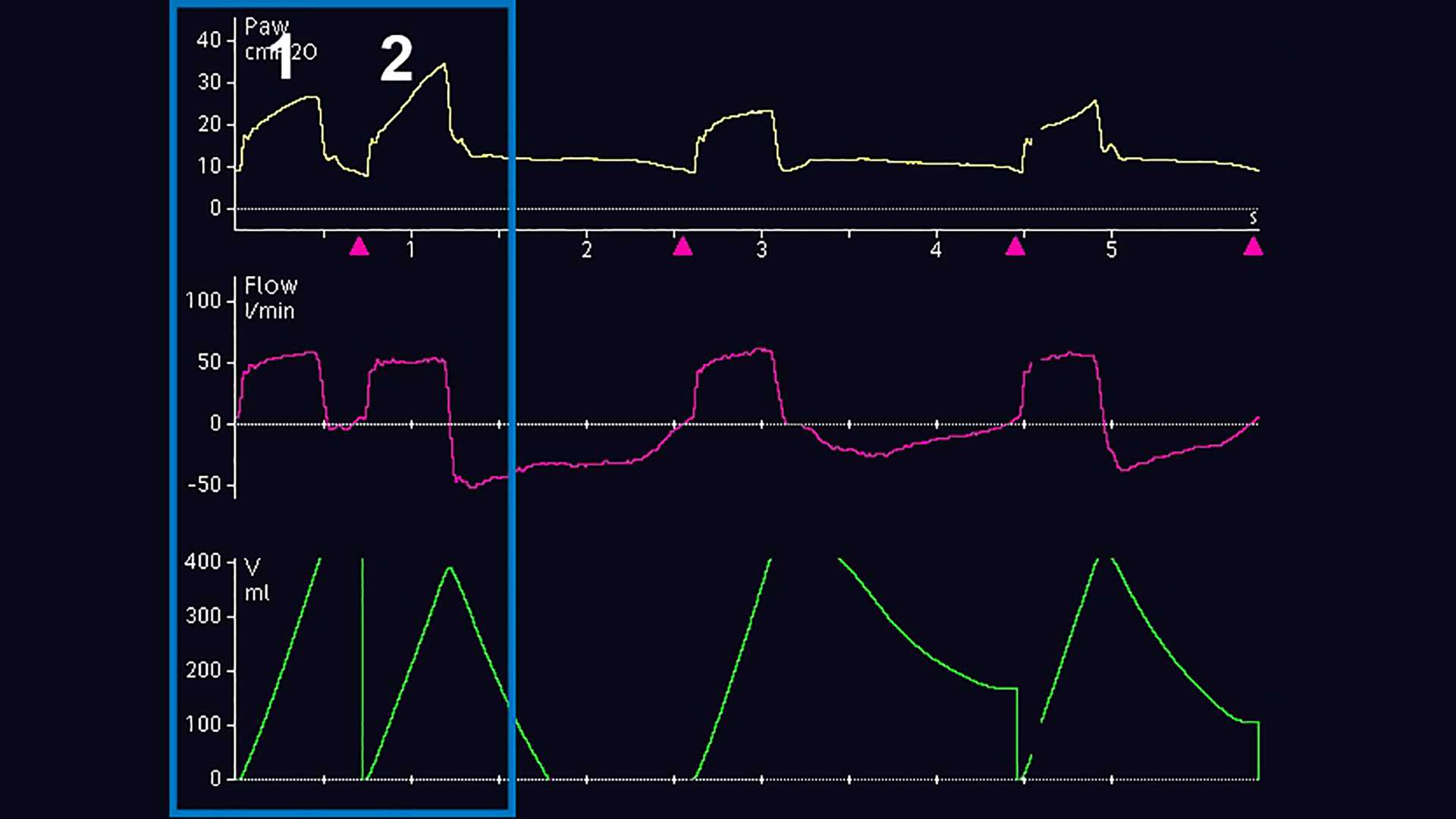
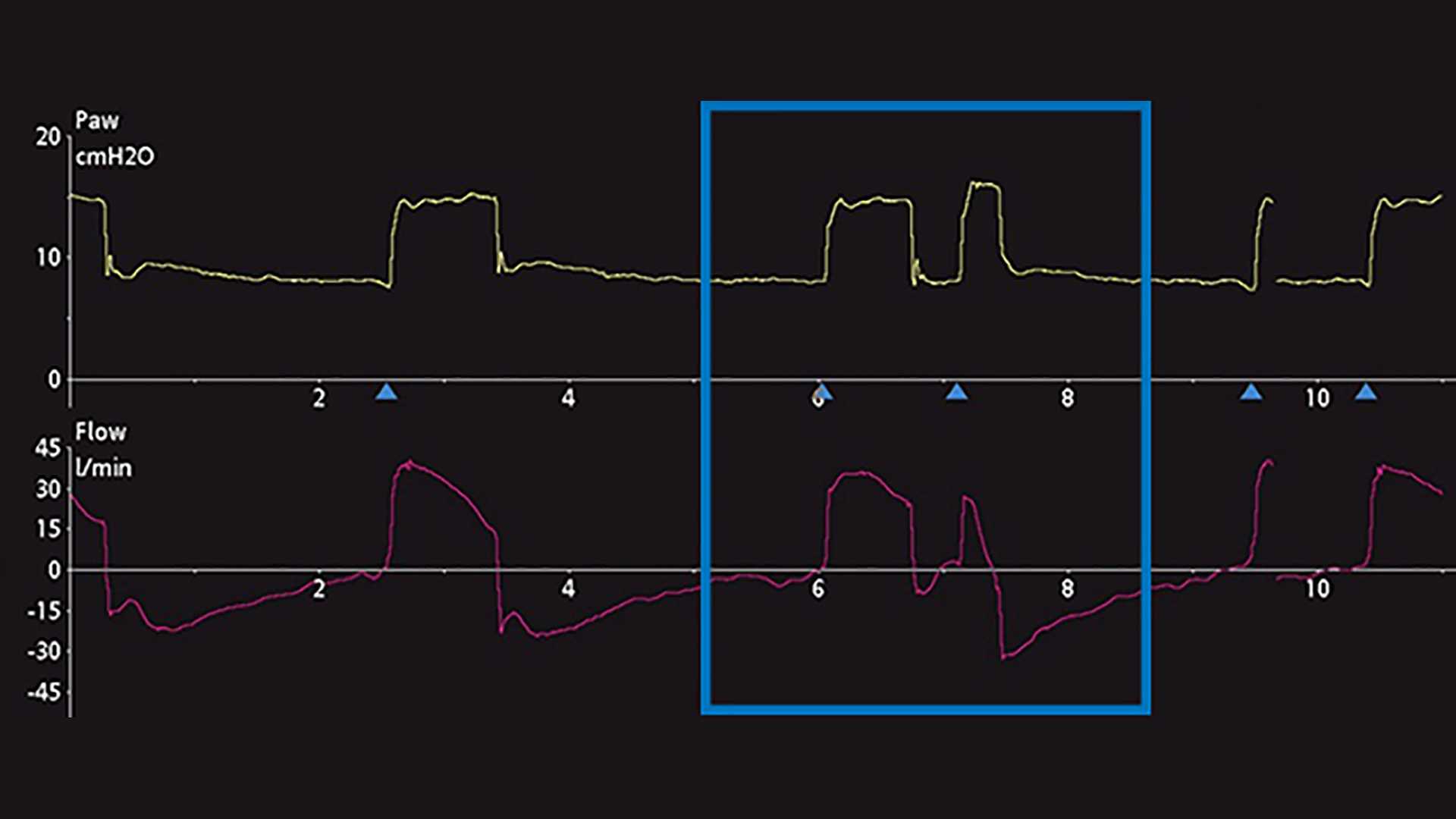
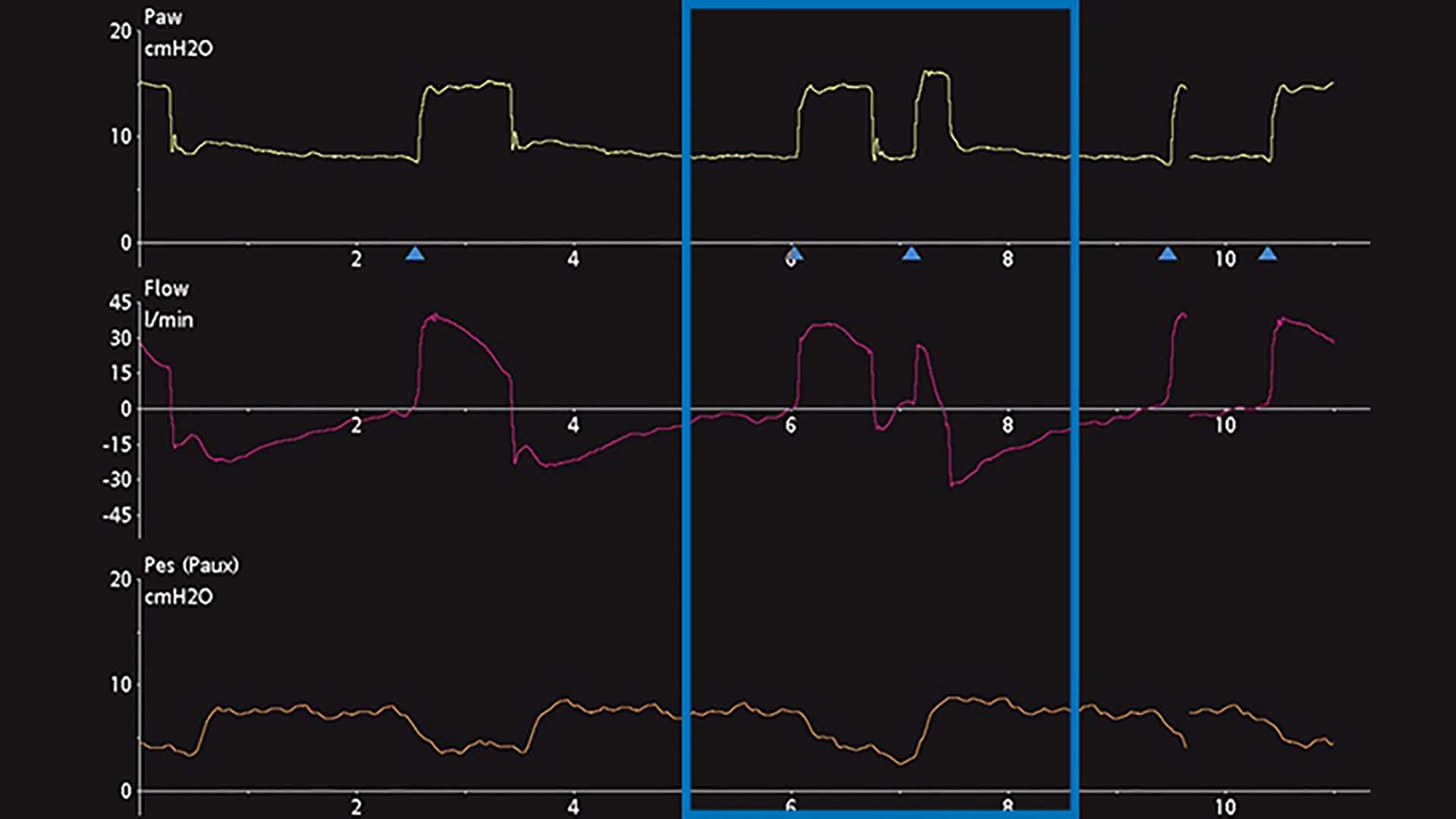
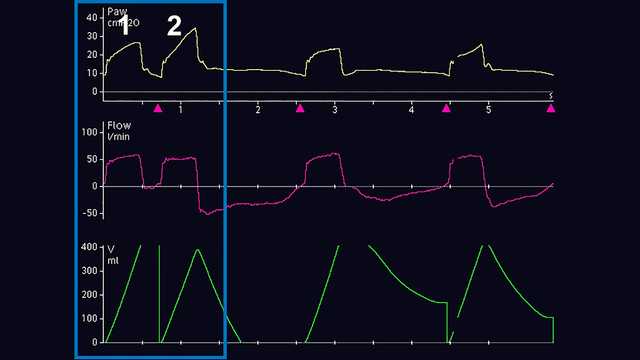
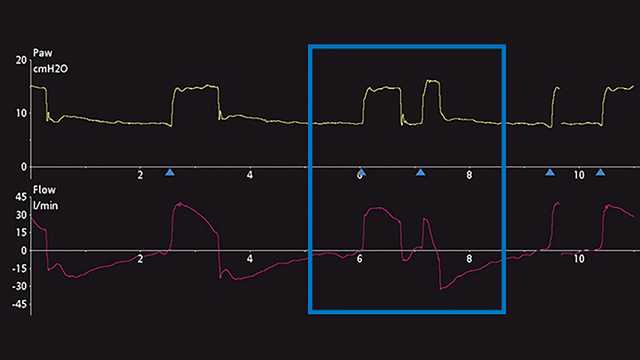
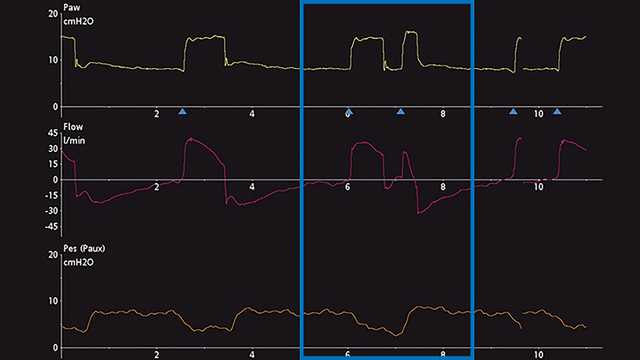
The primary method of DT diagnosis is the observation and evaluation of ventilator scalar waveforms. A scalar waveform is any variable displayed over time. Most mechanical ventilators commonly allow the display of pressure, flow and/or volume over time. To further facilitate the analysis of those waveforms, some ventilators allow the display of esophageal (approximated pleural) pressure over time. To demonstrate the steps toward proper identification of DT, screenshots of ventilator waveforms are provided below. Figure 1 displays common pressure, flow, and volume waveforms revealing the DT phenomenon during invasive ventilation. Initially, the untrained eye may not be able to diagnose this phenomenon, nor may it correctly determine the origin of the problem. Commonly mistaken for the patient actively generating a second breath (Breath 2) after delivery of a mechanically timed breath (Breath 1) or air hunger, this problem can lead to severe adverse effects related to mechanical ventilation if it continues. Therefore, closer analysis is recommended and can be performed by utilizing esophageal manometry to compare and contrast pleural pressure and the ventilator’s airway pressure and flow changes. Another example below, which shows a ventilator displaying pressure and flow time scalars, provides a subtle hint of possible DT, but may also be mistaken for an additional active inspiratory effort (Figure 2). The addition of the esophageal pressure scalar waveform (Pes‑Paux waveform) reveals that in fact a double trigger is present because of the subsequent delivery of breaths during a single active inspiratory effort (see the decrease in pleural pressure in Figure 3).
Differentiation
Differentiating and classifying the type of DT is also challenging at the bedside. Current research suggests that DT can be classified into three different types (
- Patient‑triggered (DT‑P): First triggered breath has an esophageal pressure decrease of >1 cmH2O and may be associated with a strong inspiratory effort
- Auto‑triggered (DT‑A): First triggered breath occurs earlier than the ventilator‑set time trigger, without a concomitant drop in esophageal pressure
- Ventilator‑triggered (DT‑V): First breath occurs at the ventilator‑set time trigger, without a concomitant drop in esophageal pressure
ata has shown there is often a delay in triggering in the pre‑inspiratory phase of between 0.07‑0.13 seconds (
Resolution: IntelliSync+
The most common causes for DT are the improper matching of mechanical breath I‑times to neural I‑times, and an insufficient level of pressure support with high respiratory drives (
Footnotes
- A. Not available in all markets
References
- 1. Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient‑ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32(10):1515‑1522. doi:10.1007/s00134‑006‑0301‑8
- 2. Liao KM, Ou CY, Chen CW. Classifying different types of double triggering based on airway pressure and flow deflection in mechanically ventilated patients. Respir Care. 2011;56(4):460‑466. doi:10.4187/respcare.00731
- 3. Pohlman MC, McCallister KE, Schweickert WD, et al. Excessive tidal volume from breath stacking during lung‑protective ventilation for acute lung injury. Crit Care Med. 2008;36(11):3019‑3023. doi:10.1097/CCM.0b013e31818b308b
- 4. Colombo D, Cammarota G, Alemani M, et al. Efficacy of ventilator waveforms observation in detecting patient‑ventilator asynchrony. Crit Care Med. 2011;39(11):2452‑2457. doi:10.1097/CCM.0b013e318225753c
- 5. Takeuchi M, Williams P, Hess D, Kacmarek RM. Continuous positive airway pressure in new‑generation mechanical ventilators: a lung model study. Anesthesiology. 2002;96(1):162‑172. doi:10.1097/00000542‑200201000‑00030
- 6. Parthasarathy S, Jubran A, Tobin MJ. Assessment of neural inspiratory time in ventilator‑supported patients. Am J Respir Crit Care Med. 2000;162(2 Pt 1):546‑552. doi:10.1164/ajrccm.162.2.9901024
- 7. Kallet RH, Campbell AR, Dicker RA, Katz JA, Mackersie RC. Effects of tidal volume on work of breathing during lung‑protective ventilation in patients with acute lung injury and acute respiratory distress syndrome. Crit Care Med. 2006;34(1):8‑14. doi:10.1097/01.ccm.0000194538.32158.af
- 8. Vignaux L, Vargas F, Roeseler J, et al. Patient‑ventilator asynchrony during non‑invasive ventilation for acute respiratory failure: a multicenter study. Intensive Care Med. 2009;35(5):840‑846. doi:10.1007/s00134‑009‑1416‑5