Author: Bernhard Schmitt; Mirko Belliato, MD (Pavia, Italy)
Date of first publication: 29.11.2022
Last change: 29.11.2022
English additions made in German versionAll Hamilton Medical ventilators are able to deliver noninvasive ventilation through a helmet.

NIPPV with Hamilton Medical ventilators
The turbine‑driven ventilators are able to provide higher continuous flow levels, and the air supply is fed by filtered room air (HEPA filter) with ambient humidity. Below you will find step‑by‑step instructions for using a helmet to apply NIPPV ventilation therapy to adult COVID‑19 patients with a Hamilton Medical ventilator.
NOTE! Hamilton Medical ventilators must not be used for helmet CPAP therapy. Instead, the recommendation is to use a valveless continuous flow system connected on both sides of the helmet (
Step 1: Setup and preparation
- Use a low‑compliance, dual limb breathing circuit, preferably with active humidification (can lead to significant condensation in the helmet). Do not use a coaxial circuit!
- Insert a bacterial/viral filter at the inspiratory and expiratory port of the ventilator.
- If available, activate and prepare the mainstream or sidestream CO2 sensor with the necessary airway adapters.
- Carry out all the required preoperational checks.
- Connect the flow sensor directly to one of the helmet connection ports with a 22‑mm ID connector or the calibration adapter.
- Close the second helmet connection port with a plug.
Step 2: Mode selections and alarm settings
- If available on your ventilator, select NIV mode.
- If there is no NIV option installed, consider using PCV+/PCMV.
- Adjust the alarm limits to avoid unnecessary alarms.
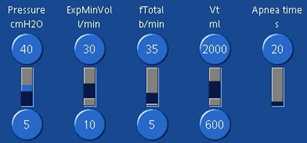
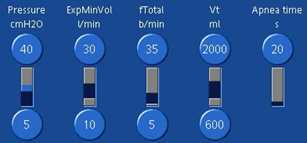
Step 3: Mode controls
ATTENTION! Two ventilated compartments in sequence = helmet + lungs.
| Pressure ramp | Set to the fastest speed possible |
| PEEP | Target PEEP + 30%‑50% Minimum PEEP = 10 cmH2O to increase helmet stiffness |
| Psupport | Target Psupport + 30%‑50% Minimum Psupport = 12 cmH2O |
| Inspiratory trigger | Start with 2 l/min and maintain as low as possible |
| ETS | Start with default ETS of 25%, monitor for cycling asynchronies and adapt accordingly |
| TI max | Set to 1.5 s to avoid late cycling |
| Oxygen | Start with Oxygen = 60% and titrate based on SpO2 Note: Single gas source (100% oxygen) may limit peak flow capacities |
Step 4: Monitoring
| Tidal volume | Between 1,000 and 1,500 ml Note: ~ 50%‑75% of the VT delivered is distributed to the helmet! (12) |
| ExpMinVol | > 25 l/min to have sufficient CO2 washout Efficiency can be monitored with PCO2 monitoring inside the helmet ‑ see Tips and tricks below. |
Tips and tricks
- Measure partial pressure of CO2 inside the helmet (PCO2h) in a “silent” part of the helmet (e.g., place the sensor directly above the inflated collar) to detect CO2 rebreathing. Use a mainstream or sidestream CO2 sensor from the ventilator or the monitoring system. PCO2h should not be above 5 mmHg/0.6 kPa.
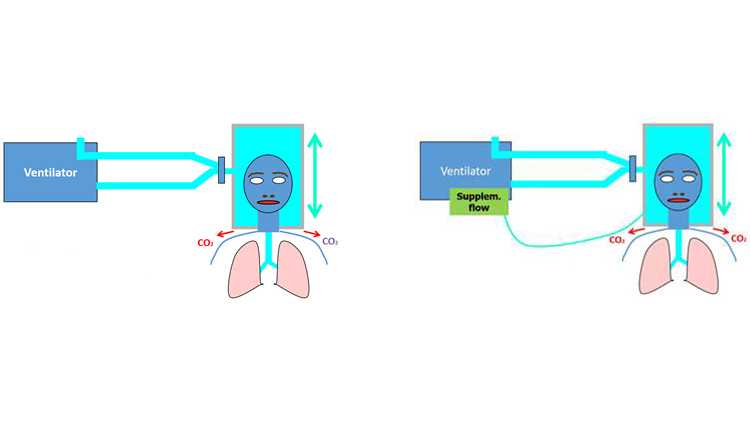
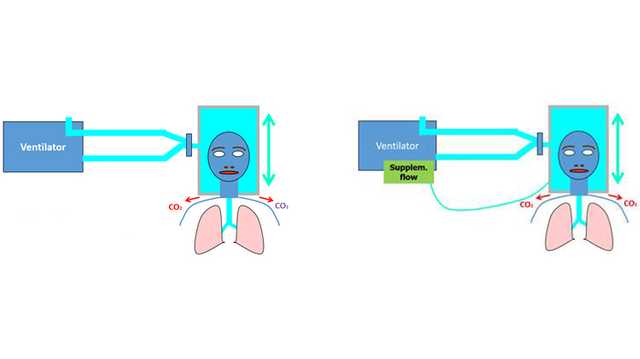
- If CO2 rebreathing is suspected, add a supplemental flow of > 10 l/min via the feeding/support port on the helmet.
- Increase pressurization by activating TRC (100%).
(Images below courtesy of Dr. Mirko Belliato, Policlinico San Matteo Pavia Fondazione IRCCS s.c. Anestesia e Rianimazione II Pavia, Italy.)
Why use a helmet for NIPPV?
When oxygen is delivered by means of a nasal catheter, mask or non‑invasive ventilation (NIV), substantial exhaled air is released into the surrounding air. This can increase dispersion of the virus, and subsequently increase the risk of nosocomial infection (
There is hope that helmet‑based ventilation may help reduce the risk of nosocomial infection: In this instance, the helmet replaces a face mask as the mode of delivering noninvasive ventilation. In a simulated environment using an ICU ventilator with a dual limb circuit and filter on the exhalation port of the ventilator, a comparison of NIPPV with a helmet and NIPPV with a face mask showed the leakage of exhaled air when ventilating with a helmet to be negligible (
Nevertheless, some experts have sounded notes of caution regarding the use of helmets. The ESICM guidelines describe them as an “attractive option” because they have “been shown to reduce exhaled air dispersion”, but the authors emphasize that they are “not certain” about the safety or efficacy of helmets in COVID‑19 patients. Therefore, they were “not able to make a recommendation regarding the use of helmet NIPPV compared with mask NIPPV” (
My Hamilton Medical ventilator doesn’t allow for a flow‑by setup...
Due to its much larger volume (always larger than the tidal volume), a helmet is similar to a semi‑closed environment such as a closed room with an air exchange system. In such an environment ‑ assuming a homogeneous distribution of CO2 ‑ the CO2 concentration depends primarily on two factors: the amount of CO2 produced by the subject (V˙CO2), and the flow of fresh gas that flushes the environment (
- The helmet is a closed environment, but ventilated
- The presence of CO2 in the helmet is inevitable
- Helmet volume does not influence rebreathing
- PCO2h (partial pressure of CO2 in the helmet) does not depend on helmet size
- Continuous high flow (minute volume) limits CO2 rebreathing
- With a total minute volume of around 30 l/min, the amount of CO2 rebreathing should be within acceptable limits
- Supplemental flow (if possible) and the (intended small) leaks help to reduce PCO2h
Disclaimer:
While the information contained herein is believed to be accurate, it does not represent an official recommendation from Hamilton Medical, nor may it substitute an opinion, assessment, or instructions provided by a trained healthcare professional
Full citations below: (
Free e‑book
Good to know! The basics of noninvasive positive pressure ventilation
Get an overview of benefits and clinical relevance of noninvasive ventilation, as well as practical information about choosing the right interface, adjusting the settings, and monitoring your patients.
Footnotes
References
- 1. Racca F, Appendini L, Gregoretti C, et al. Effectiveness of mask and helmet interfaces to deliver noninvasive ventilation in a human model of resistive breathing. J Appl Physiol (1985). 2005;99(4):1262‑1271. doi:10.1152/japplphysiol.01363.2004
- 2. Mojoli F, Iotti GA, Gerletti M, Lucarini C, Braschi A. Carbon dioxide rebreathing during non‑invasive ventilation delivered by helmet: a bench study. Intensive Care Med. 2008;34(8):1454‑1460. doi:10.1007/s00134‑008‑1109‑5
- 3. Racca F, Appendini L, Gregoretti C, et al. Helmet ventilation and carbon dioxide rebreathing: effects of adding a leak at the helmet ports. Intensive Care Med. 2008;34(8):1461‑1468. doi:10.1007/s00134‑008‑1120‑x
- 4. Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP. Effect of Noninvasive Ventilation Delivered by Helmet vs Face Mask on the Rate of Endotracheal Intubation in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA. 2016;315(22):2435‑2441. doi:10.1001/jama.2016.6338
- 5. Mojoli F, Iotti GA, Currò I, et al. An optimized set‑up for helmet noninvasive ventilation improves pressure support delivery and patient‑ventilator interaction. Intensive Care Med. 2013;39(1):38‑44. doi:10.1007/s00134‑012‑2686‑x
- 6. Taccone P, Hess D, Caironi P, Bigatello LM. Continuous positive airway pressure delivered with a "helmet": effects on carbon dioxide rebreathing. Crit Care Med. 2004;32(10):2090‑2096. doi:10.1097/01.ccm.0000142577.63316.c0
- 7. Vargas F, Thille A, Lyazidi A, Campo FR, Brochard L. Helmet with specific settings versus facemask for noninvasive ventilation. Crit Care Med. 2009;37(6):1921‑1928. doi:10.1097/CCM.0b013e31819fff93
- 8. Guan L, Zhou L, Zhang J, Peng W, Chen R. More awareness is needed for severe acute respiratory syndrome coronavirus 2019 transmission through exhaled air during non‑invasive respiratory support: experience from China. Eur Respir J. 2020;55(3):2000352. Published 2020 Mar 20. doi:10.1183/13993003.00352‑2020
- 9. Antonelli M, Conti G, Pelosi P, et al. New treatment of acute hypoxemic respiratory failure: noninvasive pressure support ventilation delivered by helmet‑‑a pilot controlled trial. Crit Care Med. 2002;30(3):602‑608. doi:10.1097/00003246‑200203000‑00019
- 10. Navalesi P, Costa R, Ceriana P, et al. Non‑invasive ventilation in chronic obstructive pulmonary disease patients: helmet versus facial mask. Intensive Care Med. 2007;33(1):74‑81. doi:10.1007/s00134‑006‑0391‑3
- 11. Moerer O, Herrmann P, Hinz J, et al. High flow biphasic positive airway pressure by helmet‑‑effects on pressurization, tidal volume, carbon dioxide accumulation and noise exposure. Crit Care. 2009;13(3):R85. doi:10.1186/cc7907
- 12. Hui DS, Chow BK, Lo T, et al. Exhaled air dispersion during noninvasive ventilation via helmets and a total facemask. Chest. 2015;147(5):1336‑1343. doi:10.1378/chest.14‑1934
- 13. Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID‑19). Intensive Care Med. 2020;46(5):854‑887. doi:10.1007/s00134‑020‑06022‑5