
Autor: Bernhard Schmitt; Mirko Belliato, MD (Pavia, Italy)
Fecha: 29.11.2022
Last change: 29.11.2022
English additions made in German versionAll Hamilton Medical ventilators are able to deliver noninvasive ventilation through a helmet.

The turbine-driven ventilators are able to provide higher continuous flow levels, and the air supply is fed by filtered room air (HEPA filter) with ambient humidity. Below you will find step-by-step instructions for using a helmet to apply NIPPV ventilation therapy to adult COVID-19 patients with a Hamilton Medical ventilator.
NOTE! Hamilton Medical ventilators must not be used for helmet CPAP therapy. Instead, the recommendation is to use a valveless continuous flow system connected on both sides of the helmet (
ATTENTION! Two ventilated compartments in sequence = helmet + lungs.
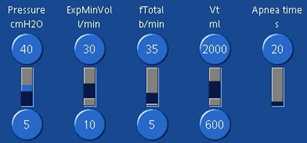
| Pressure ramp | Set to the fastest speed possible |
| PEEP | Target PEEP + 30%–50% Minimum PEEP = 10 cmH2O to increase helmet stiffness |
| Psupport | Target Psupport + 30%–50% Minimum Psupport = 12 cmH2O |
| Inspiratory trigger | Start with 2 l/min and maintain as low as possible |
| ETS | Start with default ETS of 25%, monitor for cycling asynchronies and adapt accordingly |
| TI max | Set to 1.5 s to avoid late cycling |
| Oxygen | Start with Oxygen = 60% and titrate based on SpO2 Note: Single gas source (100% oxygen) may limit peak flow capacities |
| Tidal volume | Between 1,000 and 1,500 ml Note: ~ 50%–75% of the VT delivered is distributed to the helmet! (12) |
| ExpMinVol | > 25 l/min to have sufficient CO2 washout Efficiency can be monitored with PCO2 monitoring inside the helmet - see Tips and tricks below. |
(Images below courtesy of Dr. Mirko Belliato, Policlinico San Matteo Pavia Fondazione IRCCS s.c. Anestesia e Rianimazione II Pavia, Italy.)
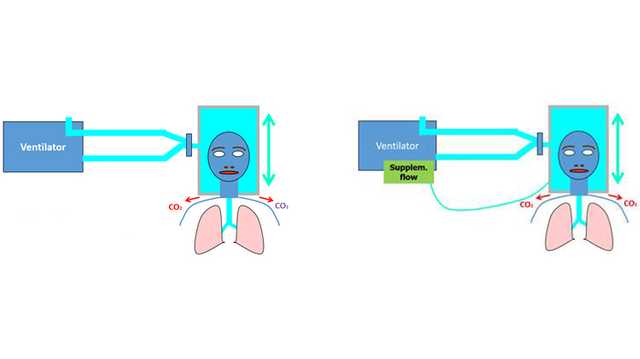
When oxygen is delivered by means of a nasal catheter, mask or non-invasive ventilation (NIV), substantial exhaled air is released into the surrounding air. This can increase dispersion of the virus, and subsequently increase the risk of nosocomial infection (
There is hope that helmet-based ventilation may help reduce the risk of nosocomial infection: In this instance, the helmet replaces a face mask as the mode of delivering noninvasive ventilation. In a simulated environment using an ICU ventilator with a dual limb circuit and filter on the exhalation port of the ventilator, a comparison of NIPPV with a helmet and NIPPV with a face mask showed the leakage of exhaled air when ventilating with a helmet to be negligible (
Nevertheless, some experts have sounded notes of caution regarding the use of helmets. The ESICM guidelines describe them as an “attractive option” because they have “been shown to reduce exhaled air dispersion”, but the authors emphasize that they are “not certain” about the safety or efficacy of helmets in COVID-19 patients. Therefore, they were “not able to make a recommendation regarding the use of helmet NIPPV compared with mask NIPPV” (
Due to its much larger volume (always larger than the tidal volume), a helmet is similar to a semi-closed environment such as a closed room with an air exchange system. In such an environment - assuming a homogeneous distribution of CO2 - the CO2 concentration depends primarily on two factors: the amount of CO2 produced by the subject (V˙CO2), and the flow of fresh gas that flushes the environment (
Disclaimer:
While the information contained herein is believed to be accurate, it does not represent an official recommendation from Hamilton Medical, nor may it substitute an opinion, assessment, or instructions provided by a trained healthcare professional
Full citations below: (
Adquiera una visión general de las ventajas y la relevancia clínica de la ventilación no invasiva, así como información práctica sobre cómo elegir la interfaz adecuada, ajustar la configuración y monitorizar a los pacientes.