Autore: David Grooms
Data: 08.07.2019

Contenuti chiave
- Le mancate sincronie tra paziente e ventilatore, dette anche "dissincronie", sono comuni nei pazienti ventilati meccanicamente.
- Una delle forme con maggiore prevalenza è il doppio trigger, generalmente dovuto a una corrispondenza non perfetta tra i tempi inspiratori dei respiri meccanici e i tempi inspiratori neurali; si tratta di una situazione particolarmente rischiosa nei pazienti con ARDS poiché può determinare l'erogazione di un volume corrente eccessivo.
- Diagnosticare il doppio trigger e distinguerne i tre diversi tipi può essere piuttosto difficile: richiede un'attenta osservazione e analisi delle curve scalari del ventilatore.
- La tecnologia attuale può aiutare i medici a evitare il doppio trigger grazie alla regolazione automatica del tempo inspiratorio in base alle esigenze del paziente.
Cos'è il doppio trigger?
La frequenza delle dissincronie è stata studiata e si stima che si verifichino almeno una volta in almeno il 50% dei pazienti sottoposti a ventilazione meccanica per oltre 24 ore. Le due dissincronie più comuni sono il trigger inefficace (o trigger mancato) e il doppio trigger (DT) (
Diagnosi e risoluzione
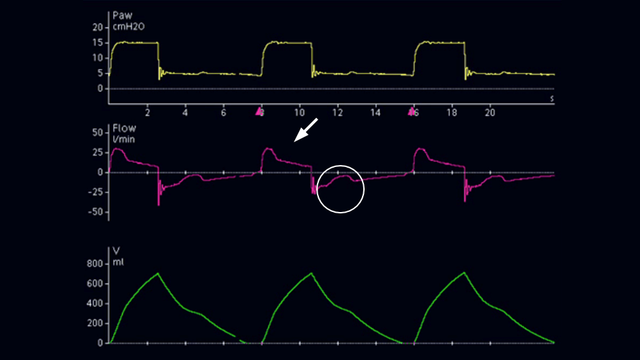
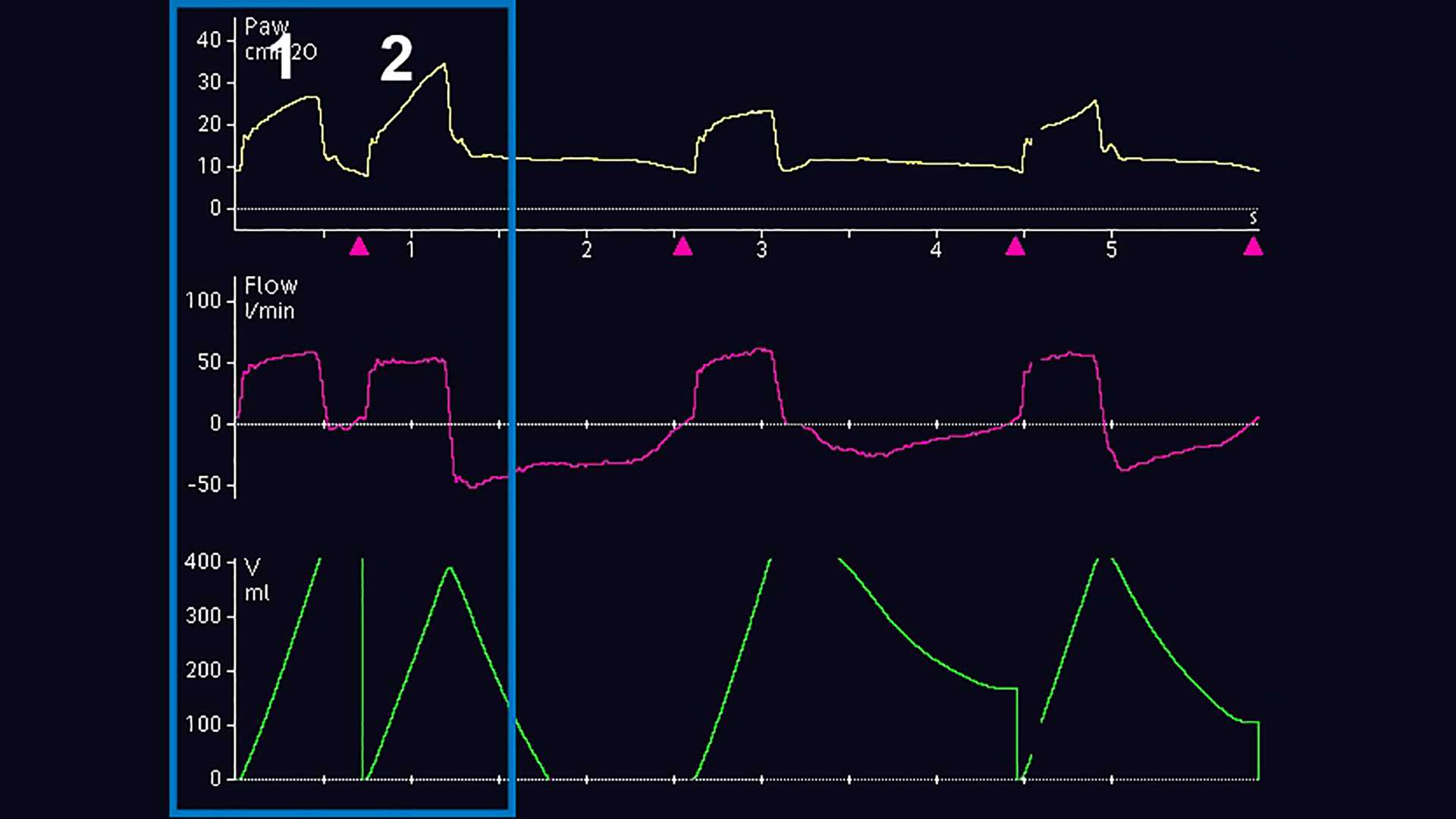
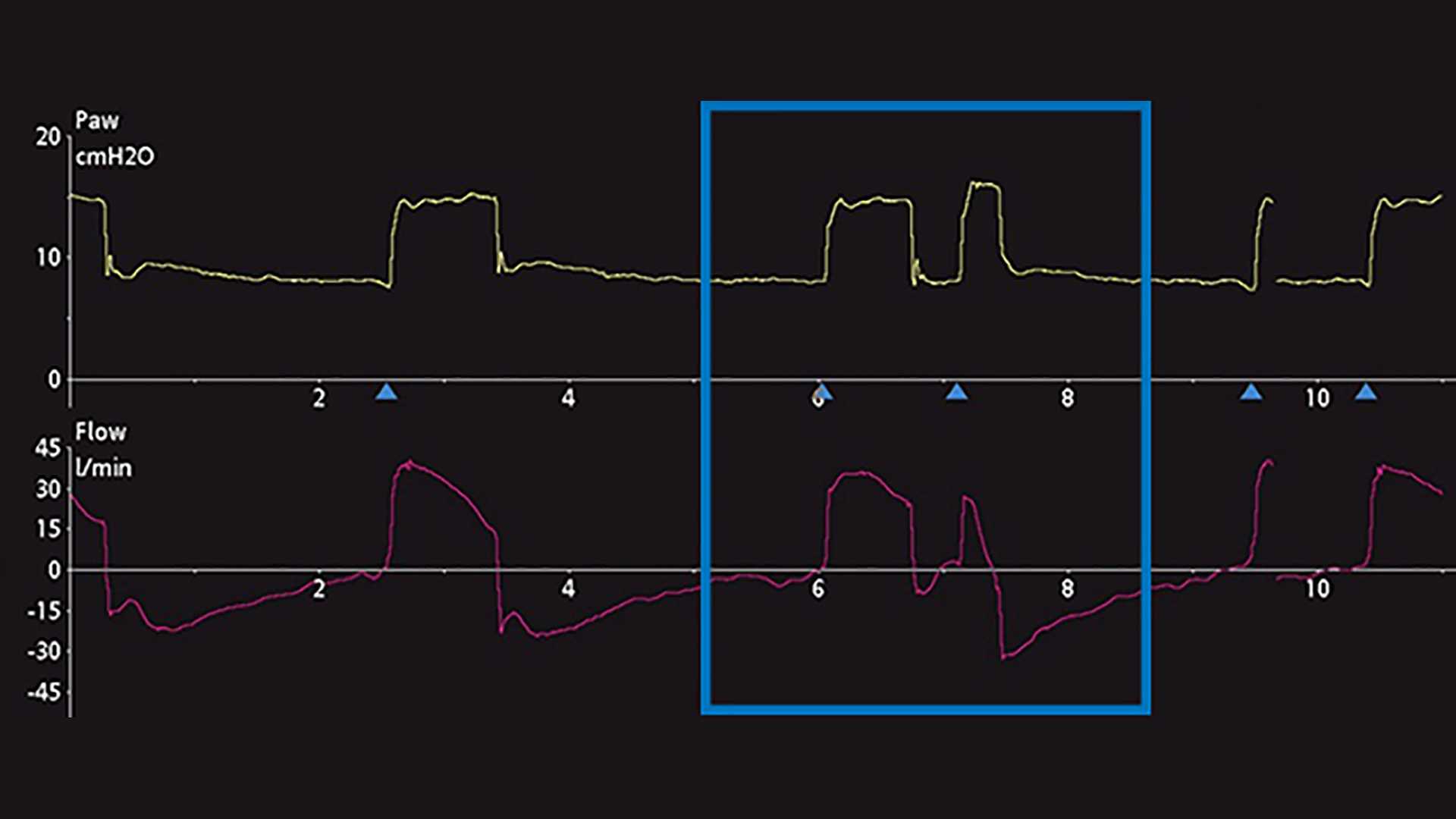
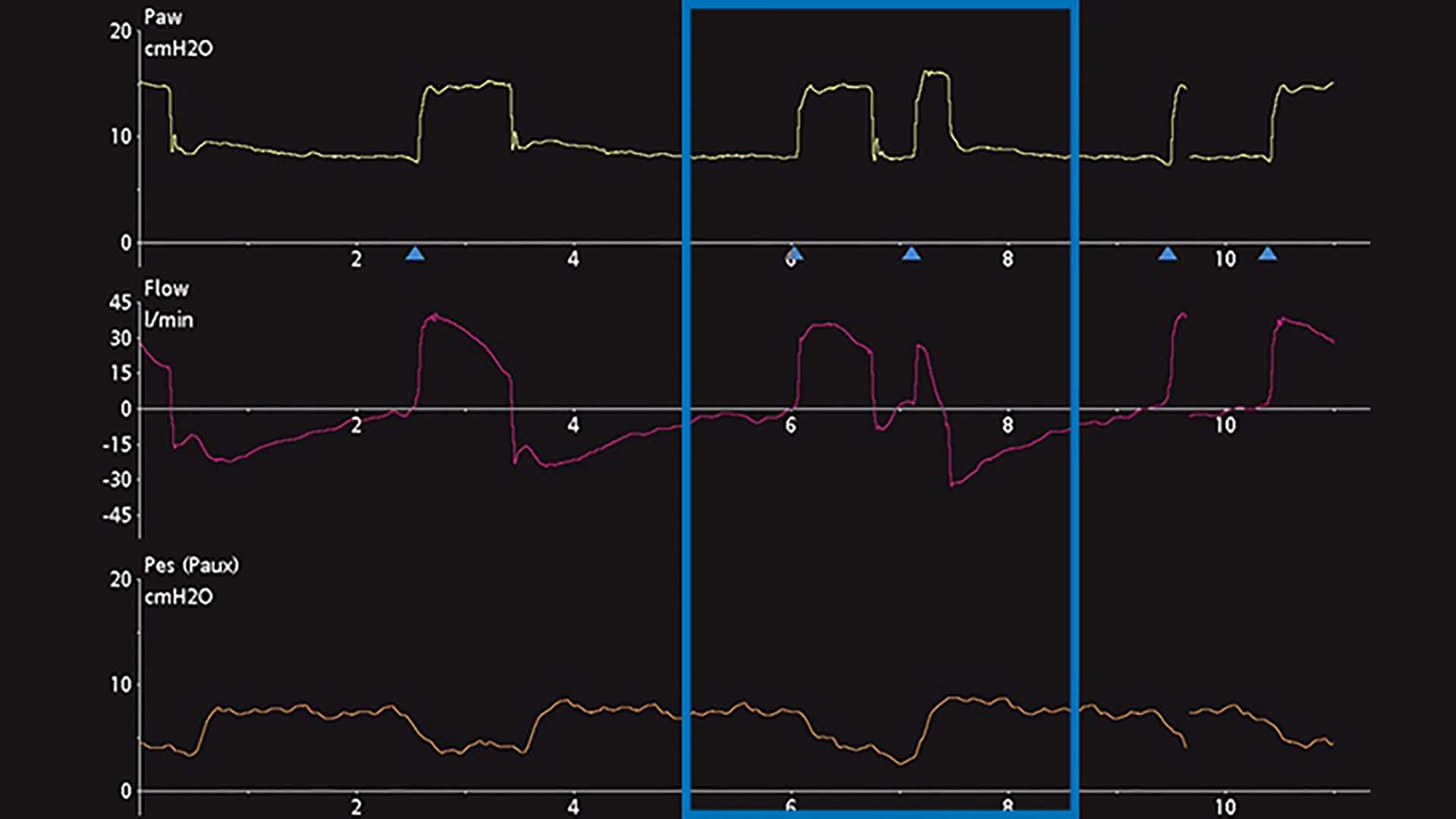
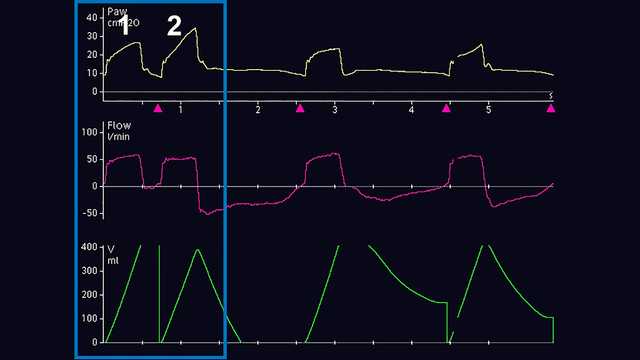
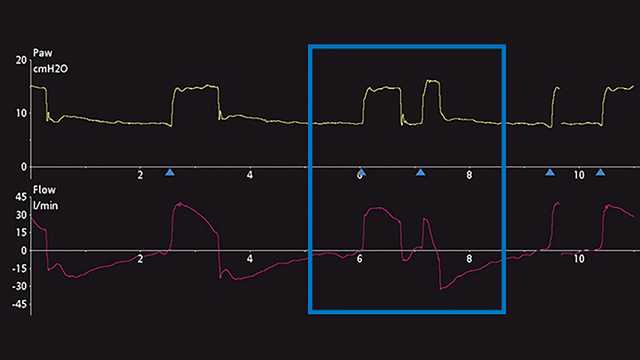
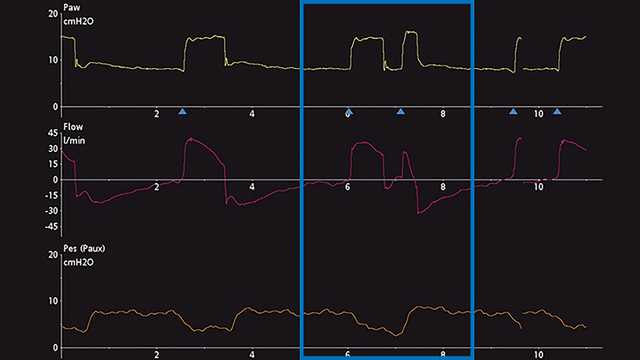
Il metodo principale per diagnosticare il doppio trigger, o DT, si basa sull'osservazione e la valutazione delle curve scalari del ventilatore. Una curva scalare è la visualizzazione di qualsiasi variabile in funzione del tempo. La maggior parte dei ventilatori meccanici consente normalmente di visualizzare l'andamento di pressione, flusso e/o volume nel tempo. Per agevolare ulteriormente l'analisi di queste curve, alcuni ventilatori consentono di visualizzare l'andamento temporale della pressione esofagea (che approssima la pressione pleurica). Per dimostrare la validità dei passaggi che permettono di identificare correttamente il DT, di seguito sono riportate alcune schermate con le curve visualizzate dal ventilatore. Nella Figura 1 sono visualizzate le normali curve di pressione, flusso e volume in cui è evidenziato il fenomeno del DT durante la ventilazione invasiva. Inizialmente, un occhio non allenato a riconoscerlo può non essere in grado di diagnosticare il fenomeno, né di individuare correttamente l'origine del problema. Spesso questa situazione viene scambiata per l'attivazione di un secondo respiro (respiro 2) da parte del paziente dopo l'erogazione di un respiro meccanico a tempo (respiro 1), oppure per "fame d'aria": questo errore può causare effetti avversi gravi legati alla ventilazione meccanica se questa prosegue senza che il problema venga risolto. È quindi consigliabile un'analisi più attenta, che si può eseguire utilizzando la manometria esofagea per confrontare la pressione pleurica, la pressione delle vie aeree del ventilatore e le variazioni di flusso. In un altro esempio mostrato di seguito, in cui sul ventilatore sono visualizzate le curve scalari di pressione e flusso in funzione del tempo, è presente un indizio di potenziale DT, che può essere scambiato anche per un ulteriore sforzo inspiratorio attivo (Figura 2). Aggiungendo la curva scalare della pressione esofagea (curva Pes/Paux) è evidente che in realtà è presente un doppio trigger a causa dell'erogazione di respiri successivi durante un singolo sforzo inspiratorio attivo (notare la diminuzione della pressione pleurica visibile nella Figura 3).
Distinzione
Anche distinguere e classificare il tipo di doppio trigger è complesso quando ci si trova al posto letto. La ricerca attuale suggerisce che sia possibile distinguere tre diversi tipi di DT (
- Innescato dal paziente (DT‑P): il primo respiro innescato corrisponde a una diminuzione della pressione esofagea > 1 cmH2O e può essere associato a uno sforzo inspiratorio intenso
- Con trigger automatico (DT‑A): il primo respiro innescato si verifica prima del trigger a tempo impostato sul ventilatore e non si ha una diminuzione concomitante della pressione esofagea
- Innescato dal ventilatore (DT‑V): il primo respiro si verifica in corrispondenza del trigger a tempo impostato sul ventilatore e non si ha una diminuzione concomitante della pressione esofagea
I dati evidenziano che spesso è presente un ritardo del trigger di 0,07‑0,13 secondi nella fase pre‑inspiratoria (
Risoluzione: IntelliSync+
Le cause più comuni di DT sono l'errata corrispondenza tra i tempi inspiratori dei respiri meccanici e i tempi inspiratori neurali, e un supporto di pressione insufficiente con drive respiratori elevati (
Note
- A. Non disponibile in tutti i mercati
Bibliografia
- 1. Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient‑ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32(10):1515‑1522. doi:10.1007/s00134‑006‑0301‑8
- 2. Liao KM, Ou CY, Chen CW. Classifying different types of double triggering based on airway pressure and flow deflection in mechanically ventilated patients. Respir Care. 2011;56(4):460‑466. doi:10.4187/respcare.00731
- 3. Pohlman MC, McCallister KE, Schweickert WD, et al. Excessive tidal volume from breath stacking during lung‑protective ventilation for acute lung injury. Crit Care Med. 2008;36(11):3019‑3023. doi:10.1097/CCM.0b013e31818b308b
- 4. Colombo D, Cammarota G, Alemani M, et al. Efficacy of ventilator waveforms observation in detecting patient‑ventilator asynchrony. Crit Care Med. 2011;39(11):2452‑2457. doi:10.1097/CCM.0b013e318225753c
- 5. Takeuchi M, Williams P, Hess D, Kacmarek RM. Continuous positive airway pressure in new‑generation mechanical ventilators: a lung model study. Anesthesiology. 2002;96(1):162‑172. doi:10.1097/00000542‑200201000‑00030
- 6. Parthasarathy S, Jubran A, Tobin MJ. Assessment of neural inspiratory time in ventilator‑supported patients. Am J Respir Crit Care Med. 2000;162(2 Pt 1):546‑552. doi:10.1164/ajrccm.162.2.9901024
- 7. Kallet RH, Campbell AR, Dicker RA, Katz JA, Mackersie RC. Effects of tidal volume on work of breathing during lung‑protective ventilation in patients with acute lung injury and acute respiratory distress syndrome. Crit Care Med. 2006;34(1):8‑14. doi:10.1097/01.ccm.0000194538.32158.af
- 8. Vignaux L, Vargas F, Roeseler J, et al. Patient‑ventilator asynchrony during non‑invasive ventilation for acute respiratory failure: a multicenter study. Intensive Care Med. 2009;35(5):840‑846. doi:10.1007/s00134‑009‑1416‑5