
Autore: Caroline Brown, Giorgio Iotti
Data: 08.07.2022
L'asincronia tra paziente e ventilatore è un'eventualità comune nei pazienti ventilati meccanicamente (1, 2).

Contenuti chiave
- L'idea di analizzare le curve di pressione e flusso per rilevare gli sforzi respiratori è stata formulata per la prima volta decenni fa, ma le evidenze sull'affidabilità di questo approccio emerse successivamente non sono determinanti.
- In uno studio recente alcuni sperimentatori, utilizzando come riferimento la curva della Pes, hanno valutato un metodo sistematico basato sull'analisi delle curve utilizzabile al posto letto per la valutazione dell'attività del paziente e dell'interazione paziente‑ventilatore.
- Il metodo delle curve ha consentito ai medici di rilevare una percentuale molto alta degli sforzi spontanei e si è dimostrato un mezzo altamente riproducibile e affidabile per identificare anche le asincronie lievi.
Una parte importante del trattamento
La mancata corrispondenza tra i tempi inspiratori ed espiratori di paziente e ventilatore può presentarsi sotto diverse forme, per esempio come ciclaggio ritardato, trigger automatico, doppio trigger o sforzo inefficace, ed è stato evidenziato che questa situazione ha un impatto sugli esiti dei pazienti (
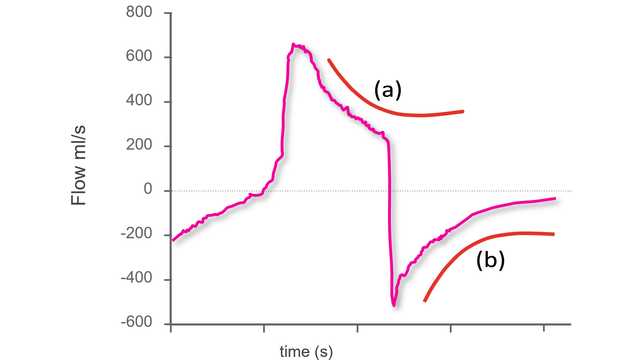
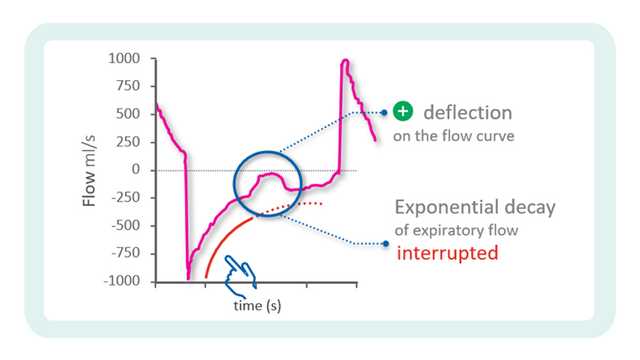
L'ipotesi di analizzare le curve di flusso e pressione delle vie aeree per rilevare gli sforzi espiratori e i relativi tempi è stata avanzata quasi trent'anni fa (
Applicazione del metodo delle curve
Un elemento chiave di questa sperimentazione è stato l'utilizzo di un metodo sistematico per l'analisi delle curve di flusso e pressione delle vie aeree, costituito da cinque principi generali e una serie di regole specifiche definite in anticipo (che chiameremo "il metodo delle curve"). Tutti i pazienti erano ventilati in modalità a supporto di pressione con un catetere esofageo posizionato. Il metodo è stato applicato alle curve del flusso e della pressione delle vie aeree ottenute tramite un sensore prossimale; la pressione esofagea (Pes) è stata utilizzata come punto di riferimento. Per ogni paziente, tre ricercatori presi da un gruppo di quattro (tre medici senior e uno specializzando) hanno analizzato solo le curve di flusso e pressione, mentre il quarto ricercatore ha analizzato sia le curve di flusso e pressione sia la curva della Pes. I respiri sono stati classificati come normalmente assistiti, a trigger automatico, a doppio trigger o sforzi inefficaci. Nel caso dei respiri normalmente assistiti, sono state valutate anche le asincronie lievi (ritardo del trigger, ciclaggio prematuro e ciclaggio ritardato).
Endpoint e risultati
L'endpoint primario era la percentuale di sforzi spontanei rilevati utilizzando il metodo delle curve. Tra gli endpoint secondari sono stati inclusi l'accordo tra il metodo delle curve e il metodo di riferimento per quanto riguarda la rilevazione di sincronie maggiori e minori, oltre all'accordo reciproco delle valutazioni eseguite con il metodo delle curve da diversi valutatori.
Sono stati registrati in totale 4.426 respiri. Utilizzando le misure di riferimento derivate dalla Pes, il 77,8% dei respiri è stato identificato come respiro correttamente rilevato dal ventilatore, il 22,1% come sforzo inefficace e lo 0,1% come respiro a trigger automatico. Con il metodo delle curve è stato possibile rilevare il 99,5% degli sforzi spontanei e tutti i respiri a trigger automatico tranne uno. L'accordo tra il metodo di riferimento e il metodo delle curve è stato molto elevato anche per la classificazione dei respiri come assistiti, a trigger automatico, a doppio trigger o sforzi inefficaci. L'indice di asincronia, calcolato come la somma dei respiri a trigger automatico, a doppio trigger e inefficaci divisa per il numero totale di respiri, è risultato pari a 5,9% e il valore ottenuto è stato il medesimo con il metodo delle curve e con quello della pressione esofagea. Il tempo di asincronia totale, calcolato come il tempo durante il quale paziente e ventilatore non erano sincronizzati diviso per il tempo di registrazione complessivo, era del 22,4%, con una componente del 92,1% dovuta alle asincronie lievi. Anche l'accordo tra i diversi operatori nella classificazione dei respiri è stato molto elevato.
In oltre il 90% dei casi, il metodo delle curve ha consentito ai ricercatori di identificare l'inizio e la fine degli sforzi respiratori con una precisione sufficiente a classificare correttamente anche le asincronie lievi (trigger ritardato, ciclaggio prematuro e ciclaggio ritardato).
Cosa ci dicono questi risultati?
Questo studio ha ottenuto alcuni importanti risultati Gli sperimentatori hanno evidenziato che il metodo delle curve consente ai medici di rilevare una percentuale molto alta degli sforzi respiratori spontanei e di valutare con precisione i tempi dell'attività del paziente. Anche nel caso di asincronie lievi, il metodo delle curve risulta altamente affidabile e riproducibile. L'importanza di questo risultato è sottolineata da un ulteriore dato rilevato dallo studio: la maggior parte del tempo di asincronia in modalità PSV era dovuto ad asincronie minori.
Non solo questi risultati dimostrano la riproducibilità del metodo delle curve (con un'elevato accordo inter‑operatore) ma evidenziano anche che una formazione nell'analisi delle curve secondo un metodo predefinito e sistematico gioca un ruolo fondamentale. Le evidenze hanno dimostrato che l'esperienza clinica nel trattamento dei pazienti ventilati meccanicamente non equivale necessariamente alla capacità di riconoscere le asincronie, che è complessivamente poco comune nei medici di terapia intensiva (
Gli autori concludono che le curve di flusso d'aria e pressione delle vie aeree misurate a livello prossimale contengono informazioni sufficienti per valutare in modo accurato l'attività del paziente e l'interazione paziente‑ventilatore, ipotizzando che si adotti un metodo di analisi sistematico adeguato, come il "metodo delle curve".
Analisi continua con IntelliSync+
La tecnologia IntelliSync®+ integrata nei ventilatori Hamilton Medical (
Citazioni complete a fondo pagina: (

Imparare a notare le più comuni asincronie: scheda di riferimento gratuita
La nostra scheda di riferimento sulle asincronie fornisce una panoramica sui tipi più comuni di asincronie, sulle loro cause e su come individuarle.
Note
- A. IntelliSync+ è disponibile come funzione opzionale sui ventilatori meccanici HAMILTON‑C6 e HAMILTON‑G5, è invece una funzione standard sul ventilatore HAMILTON‑S1.
Bibliografia
- 1. Chao DC, Scheinhorn DJ, Stearn‑Hassenpflug M. Patient‑ventilator trigger asynchrony in prolonged mechanical ventilation. Chest. 1997;112(6):1592‑1599. doi:10.1378/chest.112.6.1592
- 2. Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient‑ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32(10):1515‑1522. doi:10.1007/s00134‑006‑0301‑8
- 3. de Wit M, Miller KB, Green DA, Ostman HE, Gennings C, Epstein SK. Ineffective triggering predicts increased duration of mechanical ventilation. Crit Care Med. 2009;37(10):2740‑2745. doi:10.1097/ccm.0b013e3181a98a05
- 4. Blanch L, Villagra A, Sales B, et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 2015;41(4):633‑641. doi:10.1007/s00134‑015‑3692‑6
- 5. Fabry B, Guttmann J, Eberhard L, Bauer T, Haberthür C, Wolff G. An analysis of desynchronization between the spontaneously breathing patient and ventilator during inspiratory pressure support. Chest. 1995;107(5):1387‑1394. doi:10.1378/chest.107.5.1387
- 6. Giannouli E, Webster K, Roberts D, Younes M. Response of ventilator‑dependent patients to different levels of pressure support and proportional assist. Am J Respir Crit Care Med. 1999;159(6):1716‑1725. doi:10.1164/ajrccm.159.6.9704025
- 7. Colombo D, Cammarota G, Alemani M, et al. Efficacy of ventilator waveforms observation in detecting patient‑ventilator asynchrony. Crit Care Med. 2011;39(11):2452‑2457. doi:10.1097/CCM.0b013e318225753c
- 8. Mojoli F, Pozzi M, Orlando A, et al. Timing of inspiratory muscle activity detected from airway pressure and flow during pressure support ventilation: the waveform method. Crit Care. 2022;26(1):32. Published 2022 Jan 30. doi:10.1186/s13054‑022‑03895‑4
- 9. Ramirez II, Arellano DH, Adasme RS, et al. Ability of ICU Health‑Care Professionals to Identify Patient‑Ventilator Asynchrony Using Waveform Analysis. Respir Care. 2017;62(2):144‑149. doi:10.4187/respcare.04750
Related articles. Get a deeper look
Using waveforms to indentify asynchronies ‑ Step 1
The first step to identifying asynchronies using standard ventilator waveforms is knowing what a synchronous breath looks like during pressure‑support ventilation.
Using waveforms to identify asynchronies ‑ Step 2
In the previous issue, our Bedside tip covered the starting point for identifying asynchronies using ventilator waveforms.


