Author: Clinical Experts Group, Hamilton Medical
Date of first publication: 02.04.2020
Last change: 02.04.2020
First published: 02.06.2017 Reference 6 changed from abstract to publication, additional data added
Take‑away messages
- Driving pressure (ΔP) represents the ratio between tidal volume and respiratory system compliance, and is calculated as the difference between plateau pressure and total PEEP
- A multilevel mediation analysis of data from 2,365 ARDS patients showed that ΔP was the ventilator variable associated most strongly with hospital survival
- Results from 2,377 patients enrolled in the LUNG SAFE study showed that ΔP less than 14 cmH2O was associated with lower hospital mortality in both moderate and severe ARDS patients
- In the absence of strong recommendations based on data from prospective randomized controlled trials, it seems reasonable to aim at keeping ΔP below 14 cmH2O
- Recent evidence has shown that driving pressure was automatically limited to less than 14 cmH2O in 95% of patients ventilated in Adaptive Support Ventilation (ASV) mode
Driving pressure a substitue for lung strain
As the aerated lung has normal compliance, the reduction in respiratory system compliance is mainly due to the non‑aerated part of the lung, and can serve as an estimation of the end‑expiratory lung volume. In turn, the ratio between tidal volume and end‑expiratory lung volume represents the strain applied to the lung. Therefore, the ratio between tidal volume and respiratory system compliance ‑ also called driving pressure (ΔP) ‑ can be considered a substitute for lung strain. Driving pressure is calculated as the difference between plateau pressure and total PEEP, and can be measured quite easily using end‑inspiratory and end‑expiratory occlusions respectively.
Association between ΔP and mortality
A multilevel mediation analysis of individual pooled data from 2,365 ARDS patients included in four randomized controlled trials showed that ΔP was the ventilator variable associated most strongly with hospital survival. Any change in tidal volume or PEEP affected the outcome only when associated with a decrease in ΔP (
A large observational study aimed at better understanding the global impact of acute respiratory failure (the LUNG SAFE study) was conducted in 459 intensive care units in 50 countries around the world. Results showed that ARDS occurs in 10% of all patients admitted to the ICU, with a hospital mortality of 40% (
These results, however, should not be seen as implying that tidal volume is of no importance for lung protection. Most of the patients included in this study did indeed receive low tidal volumes. What the study does show is that when a low tidal volume is used, ΔP is an important variable to monitor for assessing the risk of hospital mortality. Although there is no data from prospective randomized controlled studies available to provide strong recommendations as to what the ΔP should be, it would seem reasonable to advocate keeping ΔP below 14 cmH2O.
How to lower driving pressure
There are several methods available for limiting ΔP, such as muscle relaxants, use of the prone position, decreasing instrumental dead space, veno‑venous extracorporeal CO2 removal, and ECMO (
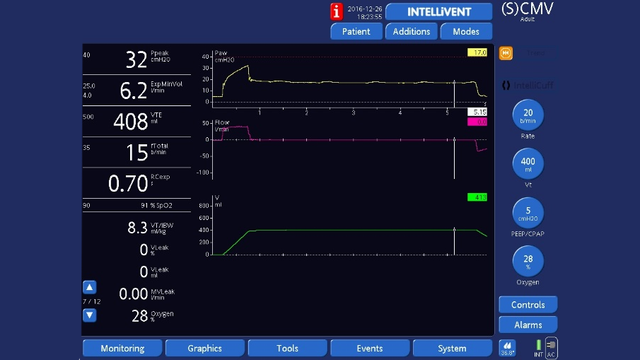
Adaptive Support Ventilation (ASV®) and INTELLiVENT®‑ASV (
Footnotes
- a. Not available in all markets
References
- 1. Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747‑755. doi:10.1056/NEJMsa1410639
- 2. Bellani G, Laffey JG, Pham T, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries [published correction appears in JAMA. 2016 Jul 19;316(3):350] [published correction appears in JAMA. 2016 Jul 19;316(3):350]. JAMA. 2016;315(8):788‑800. doi:10.1001/jama.2016.0291
- 3. Laffey JG, Bellani G, Pham T, et al. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study [published correction appears in Intensive Care Med. 2017 Nov 14;:]. Intensive Care Med. 2016;42(12):1865‑1876. doi:10.1007/s00134‑016‑4571‑5
- 4. Grieco DL, Chen L, Dres M, Brochard L. Should we use driving pressure to set tidal volume?. Curr Opin Crit Care. 2017;23(1):38‑44. doi:10.1097/MCC.0000000000000377
- 5. Borges JB, Hedenstierna G, Larsson A, Suarez‑Sipmann F. Altering the mechanical scenario to decrease the driving pressure. Crit Care. 2015;19(1):342. Published 2015 Sep 21. doi:10.1186/s13054‑015‑1063‑x
- 6. Arnal JM, Saoli M, Garnero A. Airway and transpulmonary driving pressures and mechanical powers selected by INTELLiVENT‑ASV in passive, mechanically ventilated ICU patients. Heart Lung. 2020;49(4):427‑434. doi:10.1016/j.hrtlng.2019.11.001