Author: Kathrin Seeger, ICU nurse, Hamilton Medical Clinical Application Specialist
Date of first publication: 12.06.2024
Everything healthcare professionals need to know to get started with high flow nasal cannula therapy: the flow rate, FiO2 settings, when to use HFNC, selecting the interface, and much more.

Terminology, symbols, and abbreviations
There is a range of terminology used for high flow nasal cannula (HFNC) therapy: HFNC supportive therapy, high flow therapy (HFT), nasal high flow (NHF), high flow (HF), high flow nasal cannula oxygen therapy, heated humidified high flow therapy (HHHF), high flow oxygen (HFO) therapy, and high flow oxygen therapy (HFOT). Hamilton Medical uses the term high flow nasal cannula (HFNC) therapy.
Good to know: The term HFNC refers to the therapy itself irrespective of the interface used (nasal cannula or tracheostomy connector).

Introduction
High flow nasal cannula therapy is a type of respiratory support that delivers heated and humidified gas with a controlled concentration of oxygen to your patients. This therapy has become increasingly popular for hypoxemic respiratory failure.
HFNC is used during early noninvasive management of acute respiratory failure, and has proven to be safe and effective as a noninvasive ventilation method. HFNC has been shown to be potentially useful and efficient in other applications such as major postoperative care, immunocompromised patients, for preoxygenation, or during bronchoscopy (
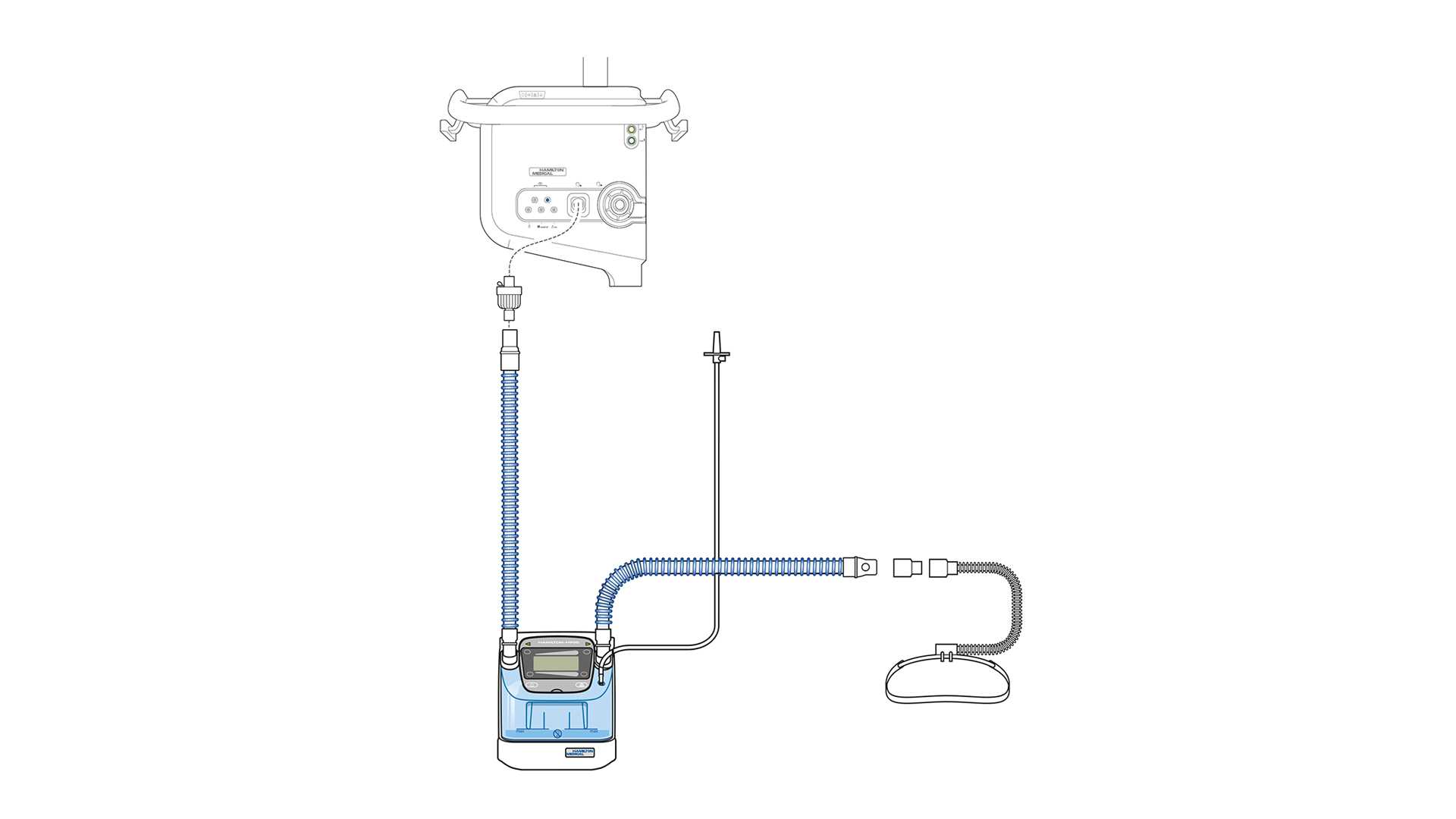
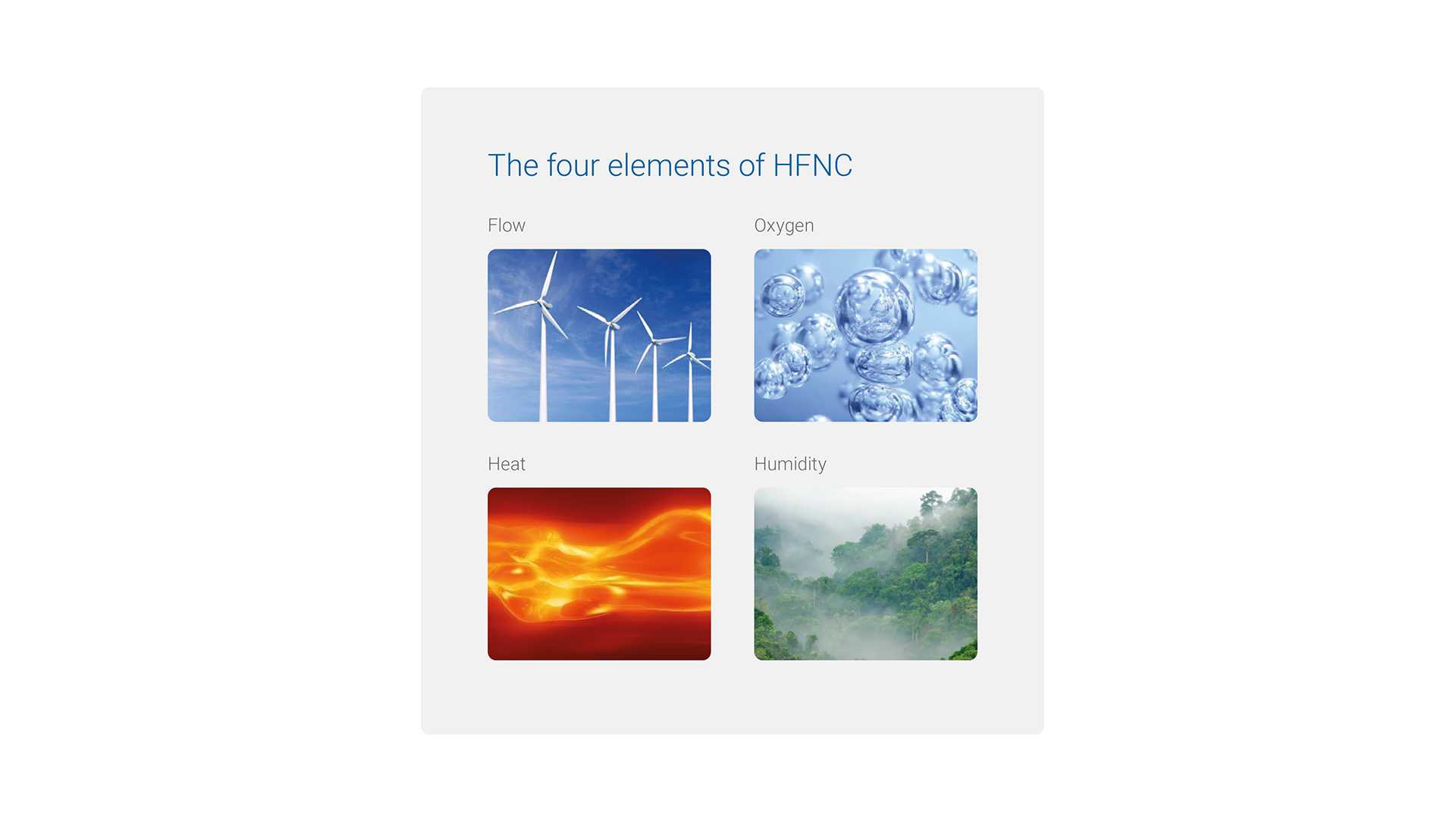
The system used to deliver HFNC requires the following components: a gas blender and flow meter, an active humidifier, a heated inspiratory circuit, and a nasal cannula or a tracheostomy connector as an interface. When we talk about high flow nasal cannula, we need to keep in mind the four elements that describe this therapy: flow, oxygen, heat, and humidity.
If we take a closer look at the meaning of each element, the advantages of using HFNC are clear:
- Flow: the higher flow rates allow you to set the inspiratory flow to adequately meet or even exceed the inspiratory demand of the patient.
- Oxygen: you can set the FiO2 more accurately within a range of 21% to 100%. However, consider escalating treatment if FiO2 of greater than 60% is needed to achieve the targeted SpO2.
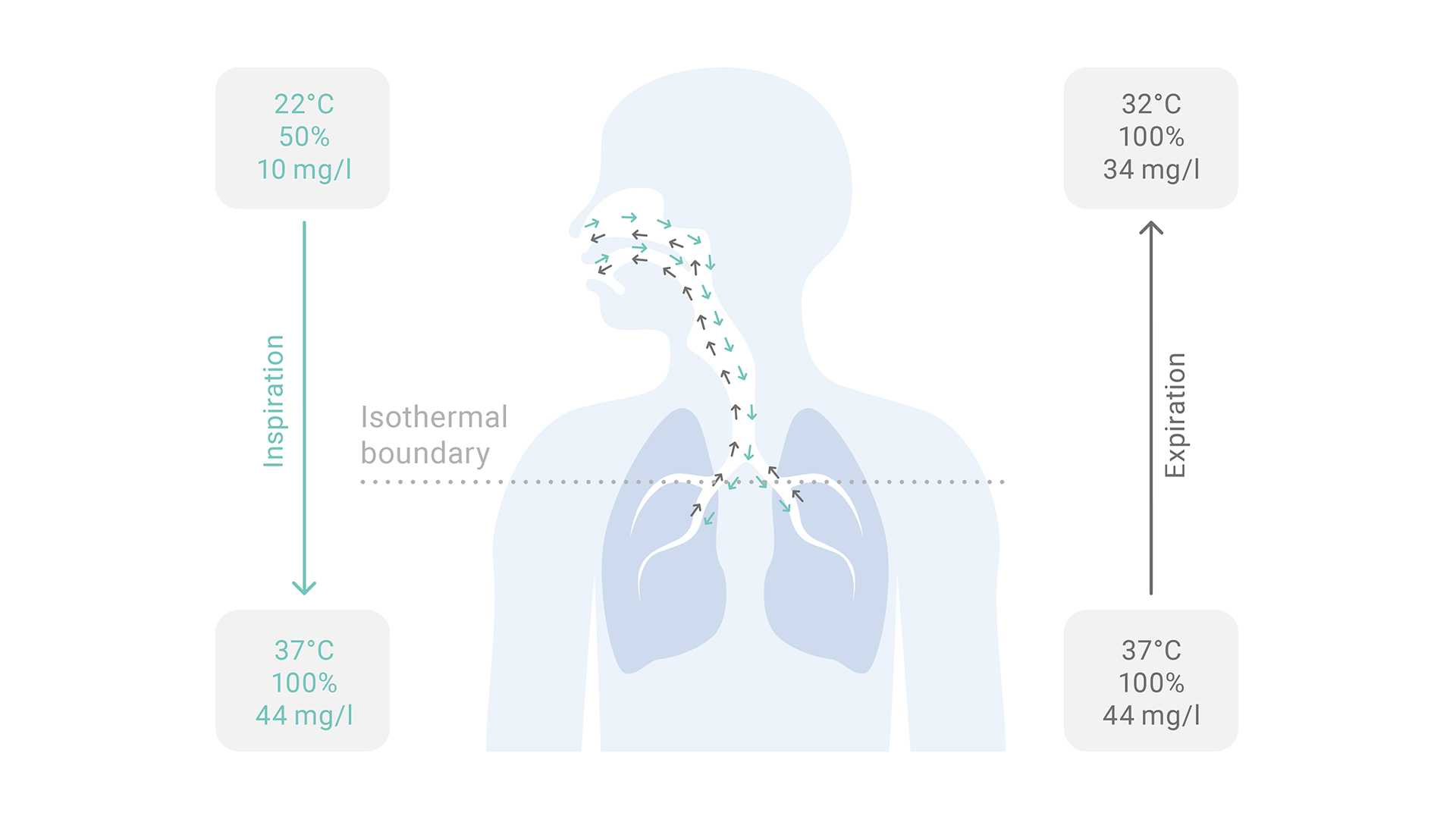
- Heat: the gas should be heated to the core body temperature of 37°C (except during NIV where the default temperature is 31°C).
- Humidity: the breathing gas is saturated close to 100% relative humidity to meet the physiologic demands.
Good to know: Did you know that the inspiratory demands of adult patients with acute respiratory failure can range from 30 l/min to more than 120 l/min?



What are the benefits of using HFNC?
We can divide the benefits of HFNC into clinical and physiologic as follows.
Clinical benefits:
- Improved patient comfort and compliance with the treatment
- Better patient tolerance due to the warmth and humidity of inspired air
- Ease of use
Physiologic benefits:
- Improved oxygenation because higher inspiratory flows mean reduced oxygen dilution
- Reduction of dead space and CO2 rebreathing compared with low flow oxygen therapy and NIV
- Reduced work of breathing associated with an improvement in respiratory rate, as well as a reduction in heart rate with a significant improvement in SpO2 measurements

How does HFNC work? Addressing the limitations of low flow
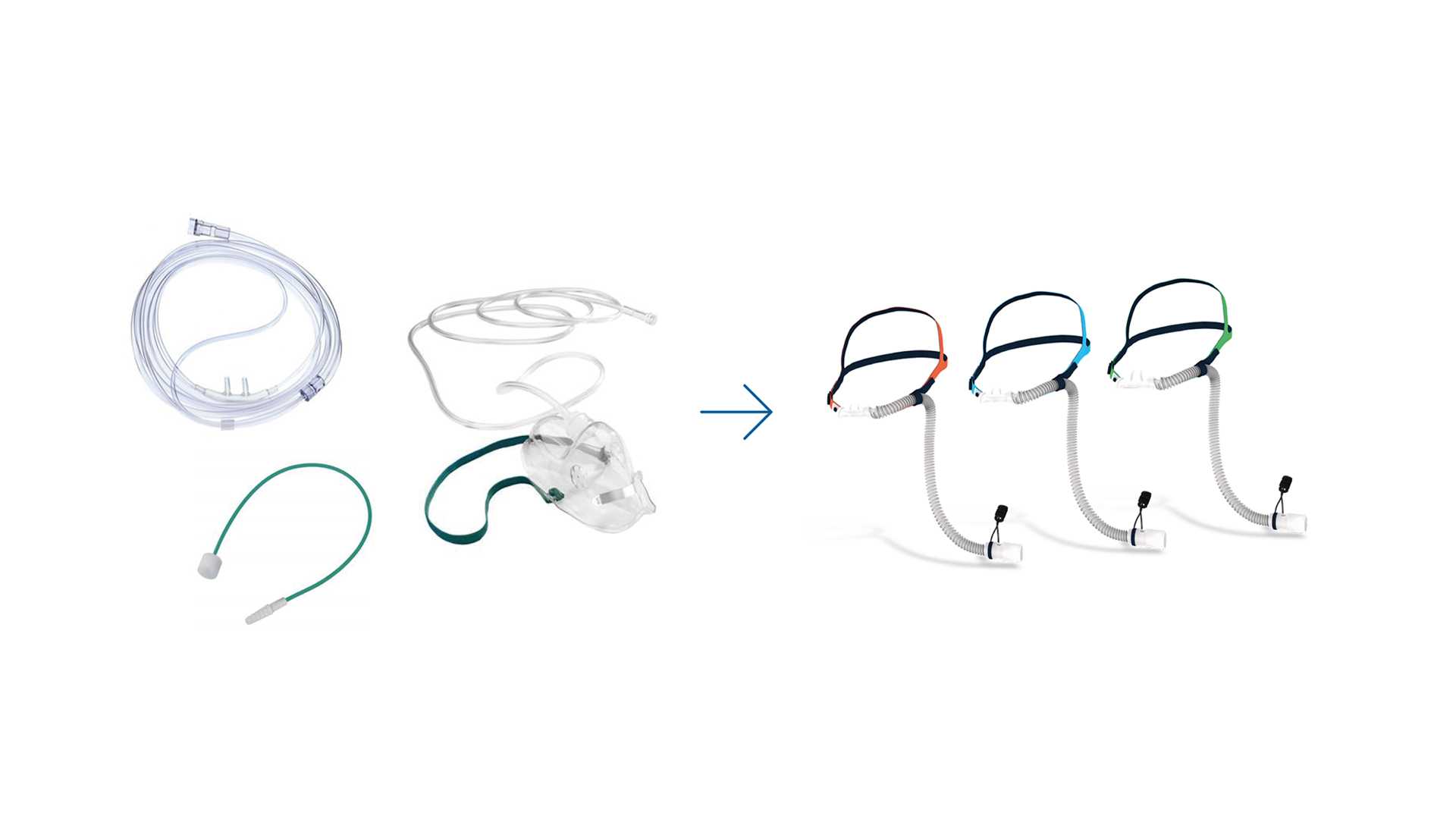
Before we dive into the working principles of high flow nasal cannula, we need to address the limitations that are typical of low flow oxygen delivery systems. This will help you better understand the beneficial effects of HFNC for your patients.
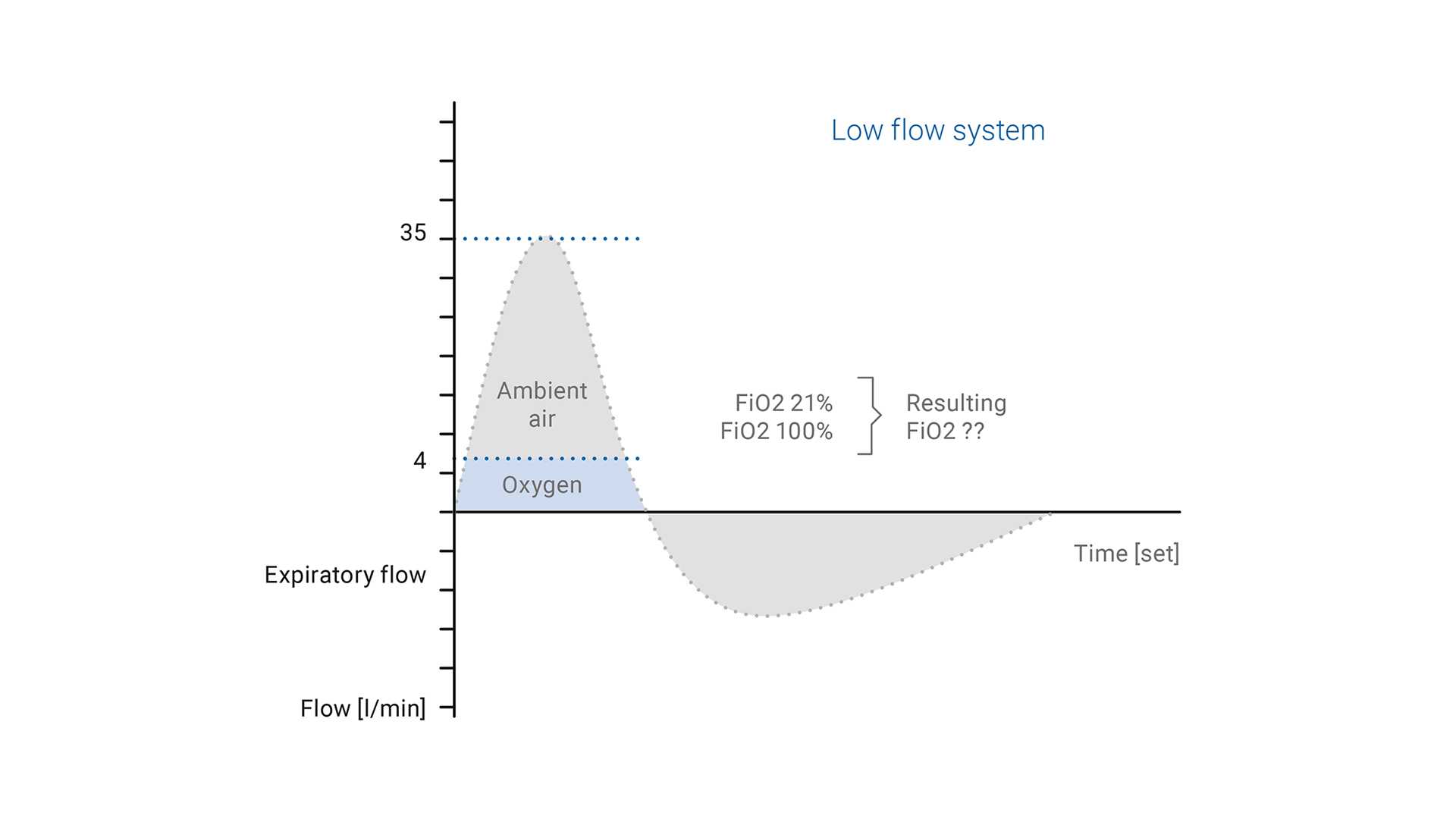
With conventional oxygen delivery devices, the peak inspiratory flow rate in acute respiratory failure patients exceeds the delivered flow of oxygen. Typical low flow systems provide supplemental O2 directly to the airway at a flow of 8 l/min or less. This O2 provided by a low flow device is always diluted with ambient air (with 21% FiO2); the result is a low and variable FiO2.
This variable FiO2 may be associated with one or more of the following: the interface used to deliver oxygen, the respiratory rate, the peak inspiratory flow and how the patient breathes (through the mouth or nose).
- Only 22% to 40% of oxygen at flow rates of up to 6 l/min in adults for low flow nasal cannulas
- Only 35% to 50% of oxygen at flow rates from 5 to 10 l/min for low flow oxygen masks
Good to know: The use of humidification is recommended when oxygen is supplied through a nasal cannula at flow rates of more than 4 l/min.

Low flow vs. high flow nasal cannula therapy
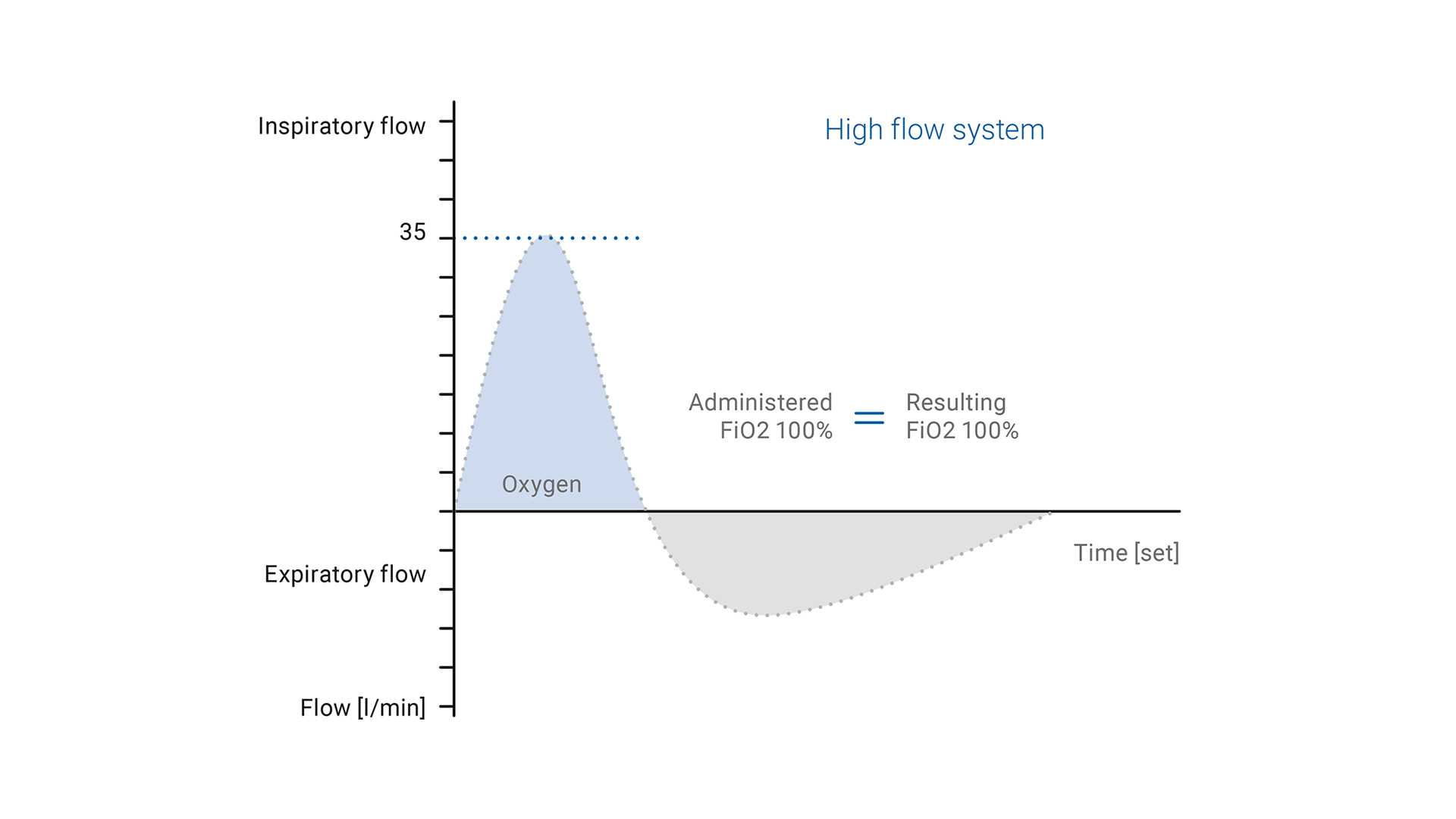
In contrast to low flow oxygen therapy, the gas flow rate and FiO2 in HFNC can be adjusted independently of one another, depending on the patient‘s inspiratory demands.
With high flow nasal cannula systems, the FiO2 is delivered more accurately and can be set from 21% to 100%.
As mentioned already, the higher flow rates are able to meet or even exceed the patient‘s peak inspiratory flow rate.
The blend of air and oxygen delivered to the patient is fully heated and humidified by the humidification chamber and the single limb heated breathing circuit. This breathing circuit contains heater wires within the tubing wall that minimize condensation.
The therapy is delivered directly into the patient‘s nostrils through a nasal cannula.
During normal inspiration, the PIF demand is 30 to 40 l/min. With high flow nasal cannula therapy, the administered FiO2 would equal the inhaled FiO2, while in the case of a low flow system, the inhaled FiO2 would be less than the administered FiO2 because it is diluted with ambient air (
For higher flows, adequate humidification is fundamental because it improves the tolerance and compliance of the treatment. HFNC systems require an active heated humidifier to achieve optimal body temperature (37°C in adults and 34°C to 37°C in pediatric patients) with a humidity output of higher than 33 mg H2O/l and close to 100% of relative humidity.
The conditions provided by HFNC promote:
- Improved lung compliance
- Improved gas distribution in the lungs
- Improved mucociliary clearance
- Decreased airway resistance
- Increased patient comfort



When to consider high flow nasal therapy
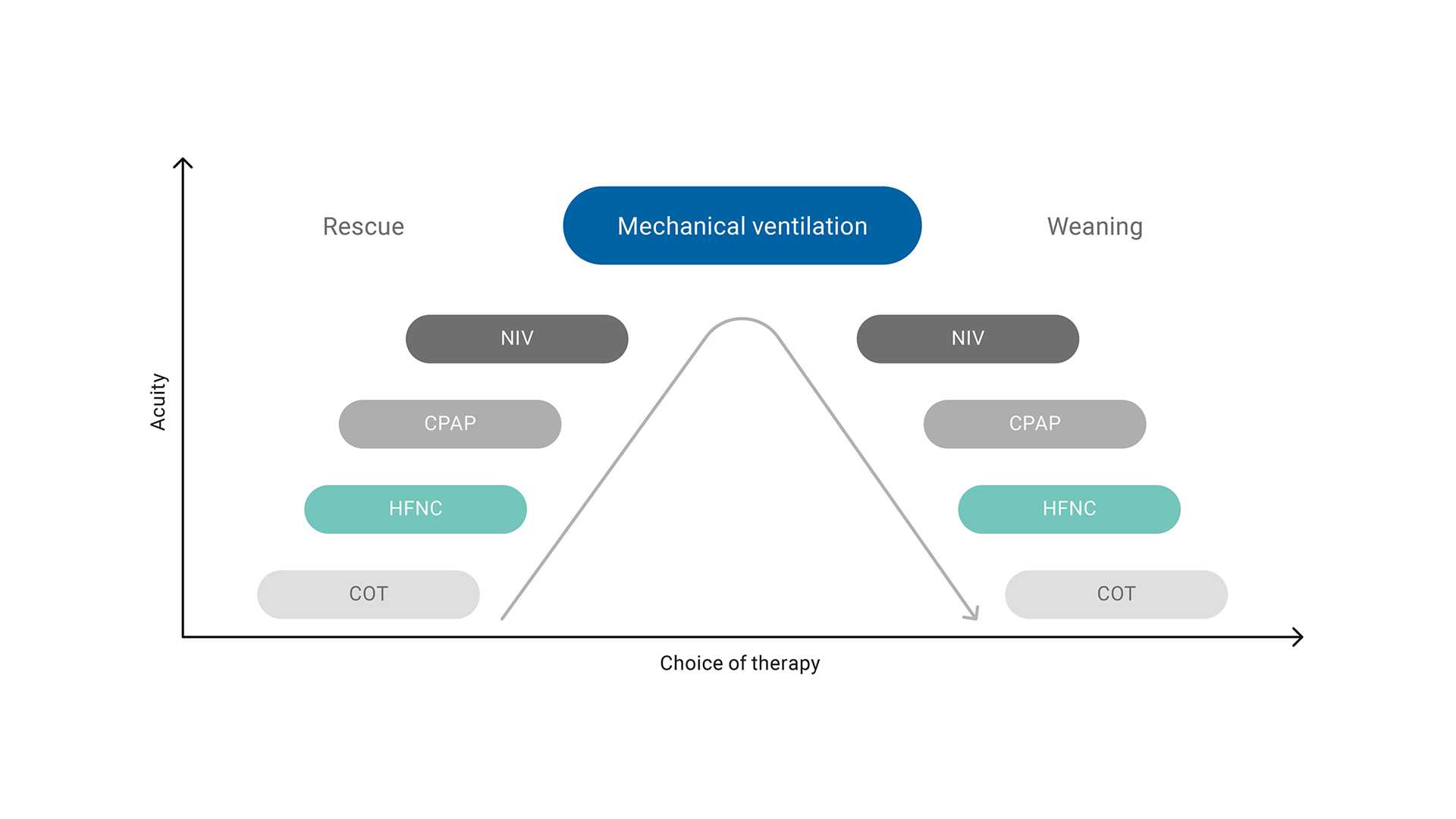
HFNC is considered the first‑line therapy for patients with acute hypoxemic respiratory failure and can be part of a treatment strategy, whether during escalation or weaning.

Recommendations for HFNC
(
| Clinical indication | Recommendation | Comments |
| Hypoxemic respiratory failure | Strong recommendation |
|
| Post‑extubation | Conditional recommendation |
|
| Post‑operative HFNC in high risk and/or obese patients following cardiac or thoracic surgery | Conditional recommendation |
|
| Peri‑intubation period | No recommendation |
|

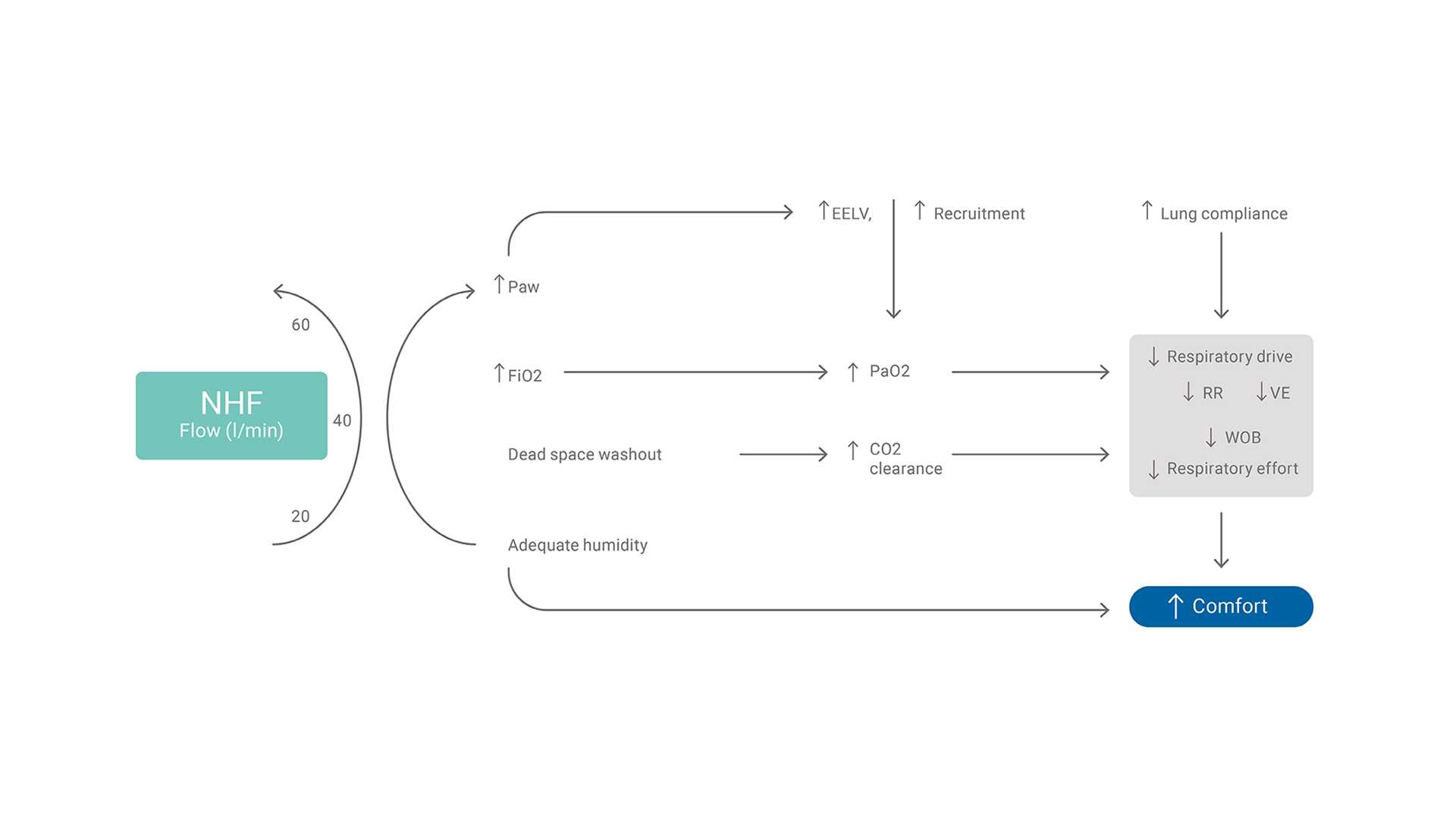
What is the clinical relevance of HFNC? The physiologic effects of high flow
Negative end‑expiratory transpulmonary pressure can cause ventilator‑induced lung injury due to atelectrauma. Studies (
- High flow generates a washout effect in the upper airways, promoting anatomic dead‑space clearance and CO2 removal
- Increases the end‑expiratory lung volume and PaO2/FiO2 ratio
- Optimal strategy for administering oxygen to hypoxic critically ill patients with high respiratory demand
- Provision of low‑level PEEP
- The therapy is delivered directly into the patient‘s nostrils through the nasal cannula
Amongst the main physiologic effects of HFNC are an increase in airway pressure and end‑expiratory lung volume (EELV), and an improvement in oxygenation. These are more evident with higher flows of around 60 to 70 l/min. However, the beneficial effects on parameters such as dead‑space washout, work of breathing, and respiratory rate may be achieved with intermediate flows (20 to 45 l/min)6.
Good to know: The physiologic effects of HFNC can be summarized as improved oxygenation, reduced work of breathing, improved lung protection and better comfort for the patient.


New It is here!
Meet our new high flow oxygen therapy device. HAMILTON‑HF90
Discover the all‑in‑one solution for high flow oxygen therapy, providing caregivers with the tools and flexibility needed to tailor treatment to each patient’s unique needs.

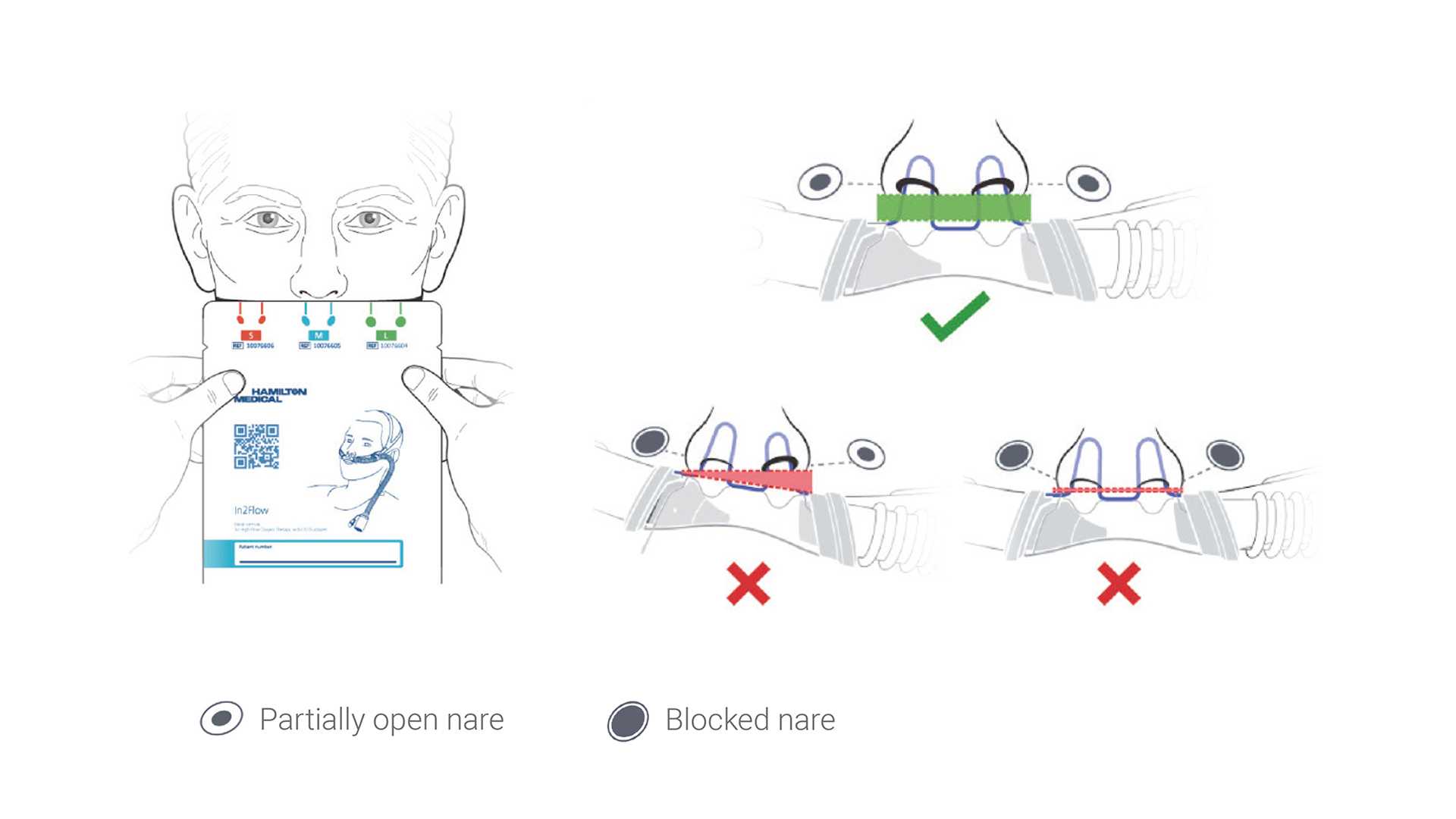
How to choose the right HFNC interface? Picking the right cannula size
The nasal cannula interface is an essential component for delivery of high flow nasal cannula therapy. In order to maintain an effective flush of CO2, it is important that the cannula does not occlude more than ~50% of the nares.
Good to know: Airway pressure increases progressively with both increasing flow rate and nasal prong‑to‑nares ratio.


How to adjust HFNC settings?
Below you can find the recommendations on how to set the flow and oxygen in adult and pediatric patients.
Important: Please note that they are only general recommendations, and every patient should be treated based on their specific medical condition.
Setting the flow in adult patients
- Set the flow initially to between 20 and 35 l/min
- The flow can be increased progressively in steps of 5 to 10 l/min if the respiratory rate fails to improve
- Increasing flows from 15 to 45 l/min triples the reduction in anatomic dead space
- To prevent intubation, choose the highest flow tolerated by the patient
(
Setting the flow in pediatric patients
Flow rates that exceed inspiratory demand can be set in patients under 24 months who tolerate flows of 1 to 2 l/kg/min (up to 20 l/min).
(
| Age | Body weight (kg) | Flow range (l/min) |
| ≤ 1 month | < 4 | 5‑8 |
| 1‑12 months | 4‑10 | 8‑20 |
| 1‑6 years | 10‑20 | 12‑25 |
| 6‑12 years | 20‑40 | 20‑30 |
| 12‑18 years | > 40 | 25‑50 |
Setting the oxygen in all patient groups
The FiO2 is the concentration of oxygen in the gas mixture delivered to the patient. In HFNC, the FiO2 should be set as follows:
- You can set the FiO2 from 21% up to 100%.
- Titrate the FiO2 to achieve the desired SpO2 (target ranges of 92%‑96% for most patients and 88%‑92% for patients with chronic respiratory disease).

How should I monitor patients on HFNC? Monitoring the effectiveness
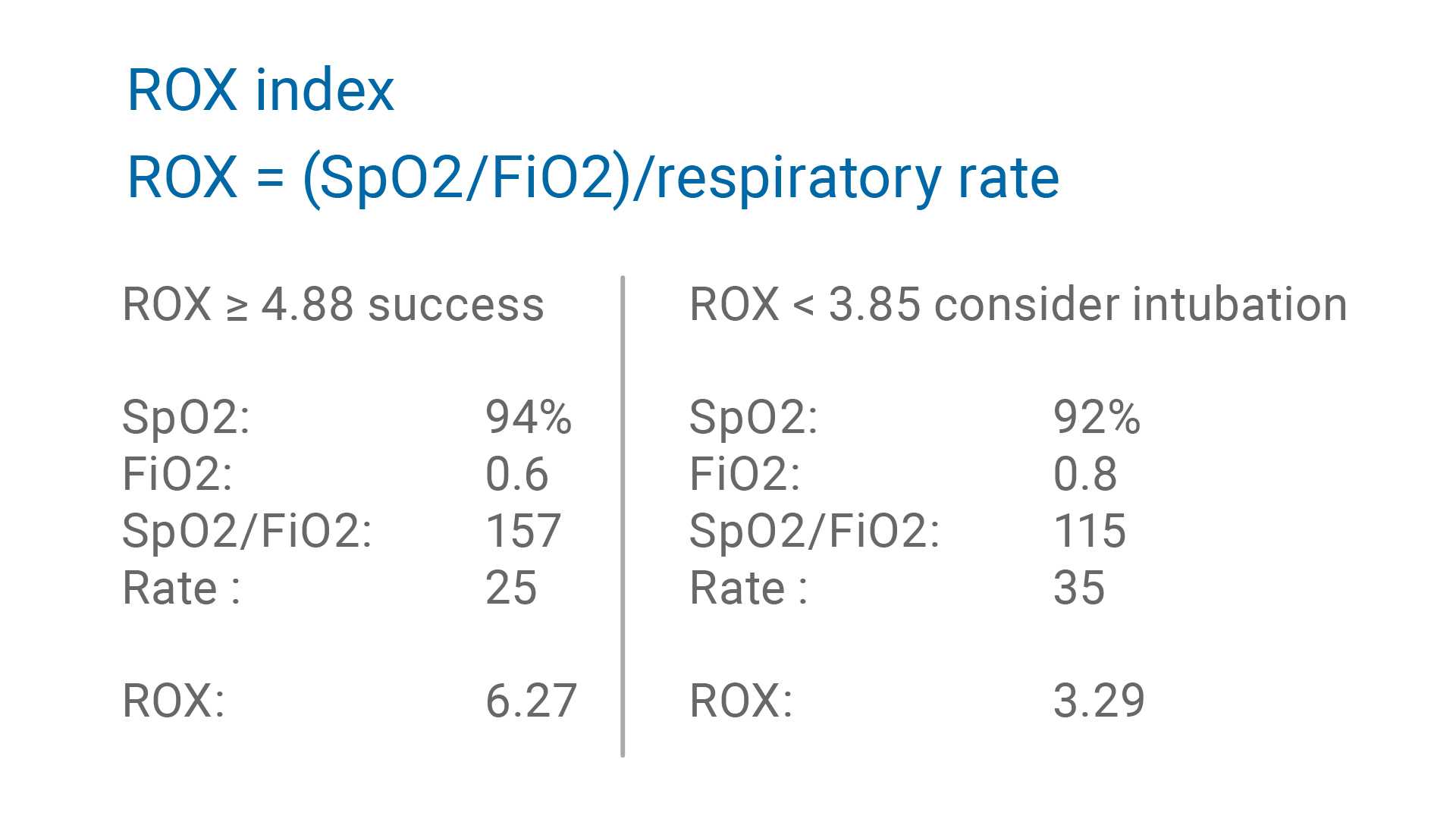
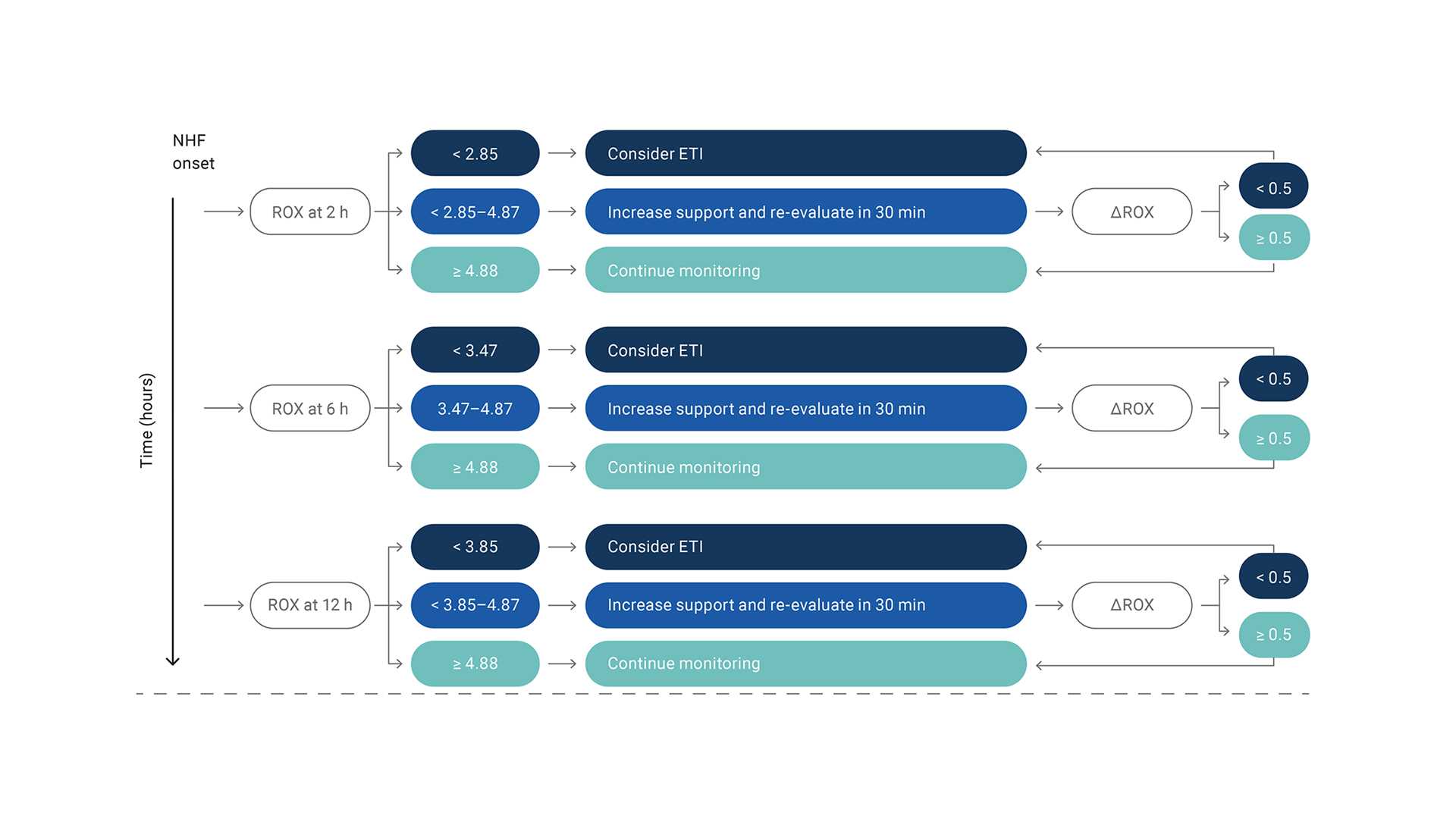
The ROX index is defined as the ratio of oxygen saturation as measured by SpO2/FiO2 to the respiratory rate. In patients with hypoxemic respiratory failure, the ROX index can be used after HFNC therapy has been initiated to help identify those who are at high risk of intubation (
ROX index ≥ 4.88 after two hours of treatment, indicates a high probability that intubation will not be necessary.
ROX index < 3.85 indicates a higher risk of treatment failure.

Recommendations for measuring the ROX index
(

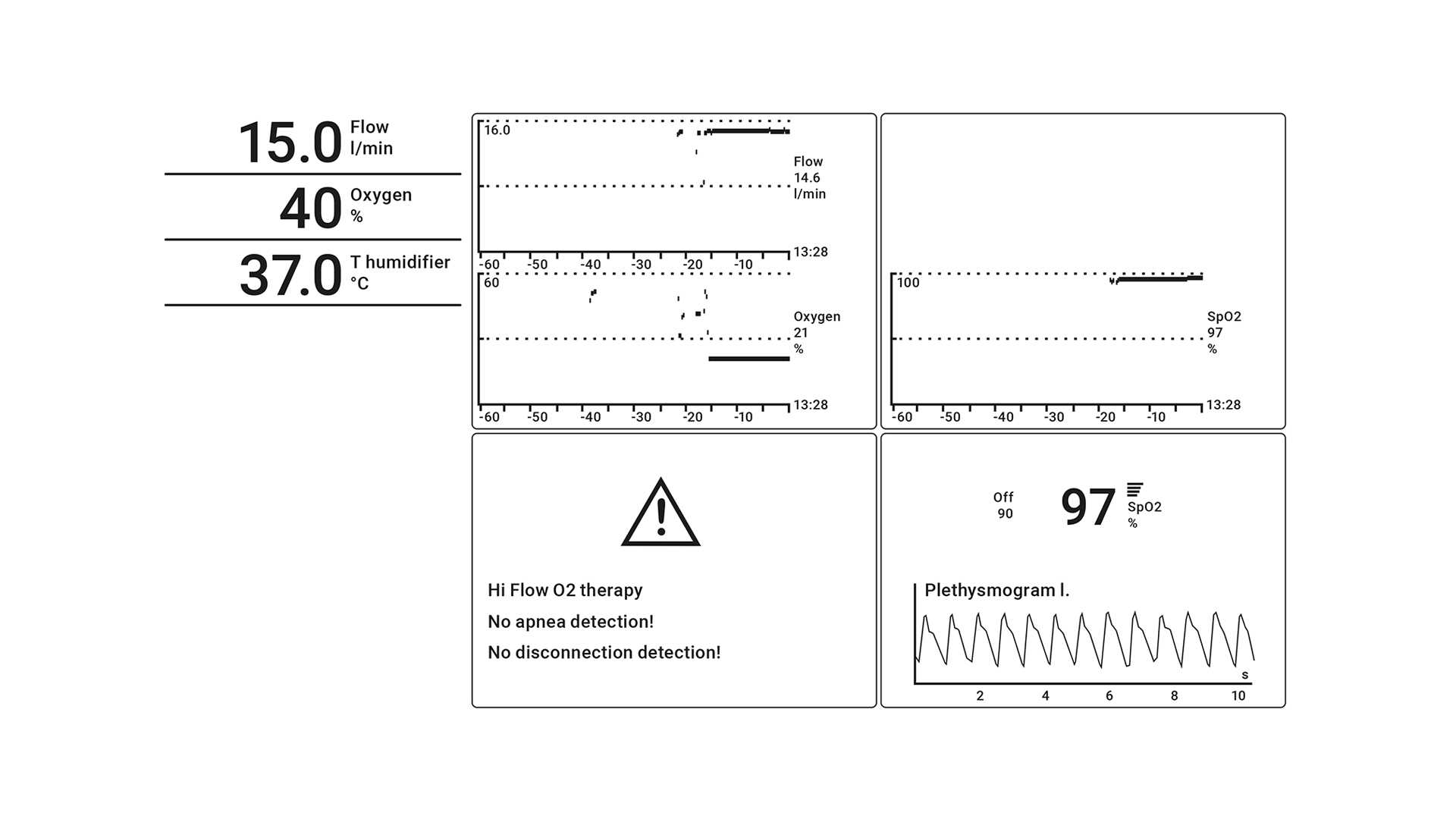
SpO2 monitoring
SpO2 is one of the most important parameters to monitor during HFNC. It indicates whether FiO2 needs to be re‑adjusted and is useful during FiO2 titration.
How to use SpO2 (
- Connect the sensor to the device and the patient
- Select the System tab
- Activate the SpO2 sensor

The monitoring shows the values of flow and oxygen over time so you can evaluate the therapy's progress.
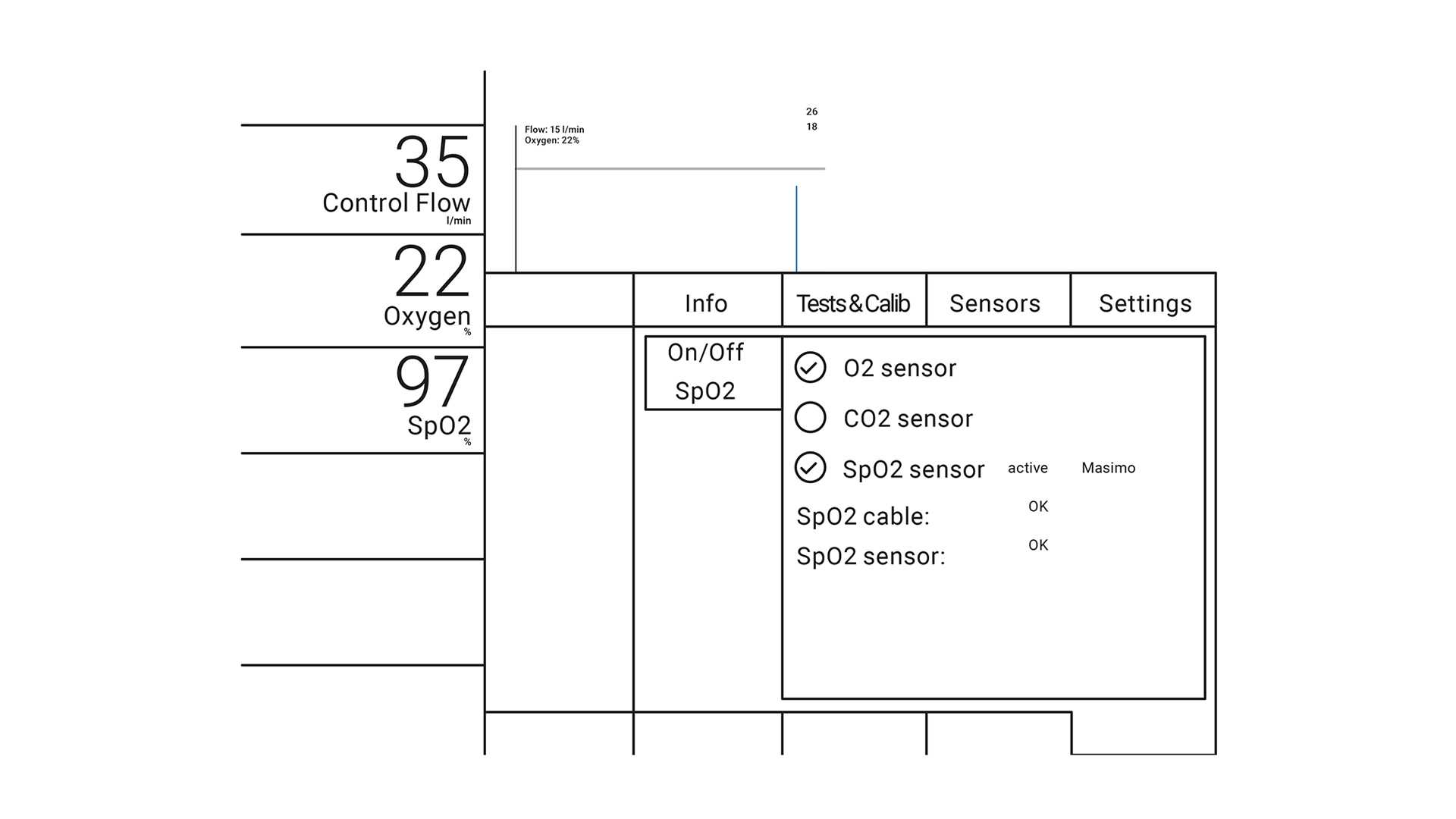
How to monitor the progress of the therapy with your Hamilton Medical ventilator:
- Main monitoring parameters
- Control flow
- Oxygen
Trending graphs:
- Select either Control Flow or Oxygen

HFNC on Hamilton Medical ventilators
Ventilators from Hamilton Medical offer high flow oxygen therapy as a standard or optional feature, in addition to continuous SpO2 and SpO2/FiO2 measurement (
It is also available on our standalone high flow oxygen therapy device, the HAMILTON‑HF90 (
We also have some exclusive offers for HFNC enthusiasts where something exciting about high flow nasal cannula therapy is waiting you.


Next steps
Dive deeper. Exclusive offers for HFNC enthusiasts
Something exciting about high flow nasal cannula therapy is waiting you. Visit the page to learn more.
Footnotes
- A. If the SpO2 option is not installed, use external patient monitoring
- A. Some features are options. Not all features/products are available in all markets. Specifications are subject to change without notice.
References
- 2. Ischaki E, Pantazopoulos I, Zakynthinos S. Nasal high flow therapy: a novel treatment rather than a more expensive oxygen device. Eur Respir Rev. 2017;26(145):170028. Published 2017 Aug 9. doi:10.1183/16000617.0028‑2017
- 3. Roca O, Riera J, Torres F, Masclans JR. High‑flow oxygen therapy in acute respiratory failure. Respir Care. 2010;55(4):408‑413.
- 4. Rochwerg B, Einav S, Chaudhuri D, et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med. 2020;46(12):2226‑2237. doi:10.1007/s00134‑020‑06312‑y
- 5. Oczkowski S, Ergan B, Bos L, et al. ERS clinical practice guidelines: high‑flow nasal cannula in acute respiratory failure. Eur Respir J. 2022;59(4):2101574. Published 2022 Apr 14. doi:10.1183/13993003.01574‑2021
- 6. Ricard JD, Roca O, Lemiale V, et al. Use of nasal high flow oxygen during acute respiratory failure. Intensive Care Med. 2020;46(12):2238‑2247. doi:10.1007/s00134‑020‑06228‑7
- 7. Drake MG. High‑Flow Nasal Cannula Oxygen in Adults: An Evidence‑based Assessment. Ann Am Thorac Soc. 2018;15(2):145‑155. doi:10.1513/AnnalsATS.201707‑548FR
- 8. Kwon JW. High‑flow nasal cannula oxygen therapy in children: a clinical review. Clin Exp Pediatr. 2020;63(1):3‑7. doi:10.3345/kjp.2019.00626
- 9. Roca O, Messika J, Caralt B, et al. Predicting success of high‑flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J Crit Care. 2016;35:200‑205. doi:10.1016/j.jcrc.2016.05.022
Related articles. Get a deeper look

How to set high flow oxygen therapy
High flow oxygen therapy combines several physiologic effects.

High flow therapy in COVID‑19 pneumonia
High‑flow therapy (HFT) is a non‑invasive form of respiratory support that can lower the intubation rate and mortality in patients with acute hypoxemic respiratory failure (AHRF) (1). Driven by concerns about the exposure of healthcare workers, initial recommendations discouraged the use of HFT in COVID‑19 patients (2, 3).

Can we predict the failure of HFNC in patients with acute hypoxemic respiratory failure?
The coronavirus pandemic has stretched many hospitals’ resources to the limit. Patients are requiring respiratory support on an unprecedented scale and a possible ‑ or in some cases very real ‑ shortage of ventilators is forcing institutions to weigh up the risks and benefits of alternative forms of therapy.

Can I measure work of breathing for patient and ventilator?
Work of breathing (WOB) represents the integral of the product of volume and pressure. It represents the energy associated with a given VT at a given pressure (spontaneous, mechanical, or both).