Author: Clinical Experts Group, Hamilton Medical
Date of first publication: 14.12.2017
Last change: 13.07.2020
More information on physiological effects; initial flow setting lowered from 60 to 30High flow oxygen therapy combines several physiologic effects.

Personalized instead of standardized settings
The physiologic effects of HFOT are improved oxygenation, reduced inspiratory effort and work of breathing, improved lung mechanics, increased end‑expiratory lung volumes (EELV), probably due to the positive end‑expiratory pressure (PEEP) effect, increased carbon dioxide (CO2) clearance by washout of anatomic dead space, and improved comfort (
The PEEP effect and the decrease in in respiratory rate are flow‑dependent and better with higher flow rates (
Initial settings and adjustments
Flow: While many of the targeted physiologic variables show the most benefit at higher flows, patient comfort and compliance to therapy are key factors that should not be ignored. The set flow should take into consideration the severity of the patient’s condition.
Although there is no standard way to set the flow, an approach now used frequently in clinical practice is to initiate with a minimum flow of 30 l/min, and monitor dyspnea and the respiratory rate. If there is no improvement, the flow can be titrated according to patient comfort. You can increase it in increments of 10 l/min up to 60 l/min, and monitor the patient’s clinical condition. Note that any discomfort is usually due to the velocity of gas rather than the flow itself, and may be eased by using a large‑bore cannula.
Temperature: In order to optimize the humidification effect, the temperature should be set at 37°C.
Oxygen: Oxygen is adjusted to maintain SpO2 within target ranges of 92%‑96% for most patients and 88%‑92% for patients with chronic respiratory disease (
This bedside tip is based on the example of high flow oxygen therapy with Hamilton Medical ventilators, however the information applies to the use of high flow oxygen therapy in general.
Full citations below: (
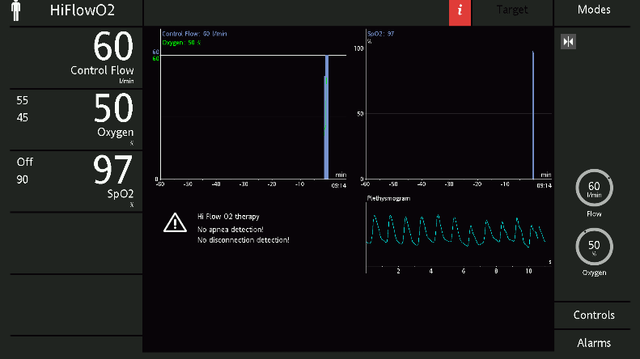

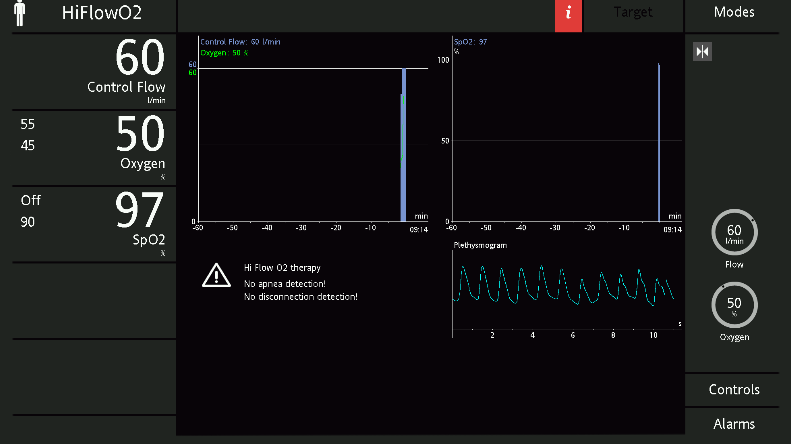
High flow oxygen therapy on Hamilton Medical ventilators
Ventilators from Hamilton Medical offer high flow oxygen therapy as a standard or optional feature, in addition to continuous SpO2 and SpO2/FiO2 measurement (
It is also available on our standalone high flow oxygen therapy device, the HAMILTON‑HF90 (

Free e‑book
The basics of high flow nasal cannula therapy
Our e‑book on high flow nasal cannula therapy gives you an overview of the working principles and clinical benefits, as well as practical information about choosing the right interface, adjusting the settings, and monitoring your patients.
Footnotes
- A. Some features are options. Not all features/products are available in all markets. Specifications are subject to change without notice.
References
- 1. Mauri T, Turrini C, Eronia N, et al. Physiologic Effects of High‑Flow Nasal Cannula in Acute Hypoxemic Respiratory Failure. Am J Respir Crit Care Med. 2017;195(9):1207‑1215. doi:10.1164/rccm.201605‑0916OC
- 2. Goligher EC, Slutsky AS. Not Just Oxygen? Mechanisms of Benefit from High‑Flow Nasal Cannula in Hypoxemic Respiratory Failure. Am J Respir Crit Care Med. 2017;195(9):1128‑1131. doi:10.1164/rccm.201701‑0006ED
- 3. Mauri T, Alban L, Turrini C, et al. Optimum support by high‑flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43(10):1453‑1463. doi:10.1007/s00134‑017‑4890‑1
- 4. Parke RL, Bloch A, McGuinness SP. Effect of Very‑High‑Flow Nasal Therapy on Airway Pressure and End‑Expiratory Lung Impedance in Healthy Volunteers. Respir Care. 2015;60(10):1397‑1403. doi:10.4187/respcare.04028
- 5. Pisani L, Fasano L, Corcione N, et al. Change in pulmonary mechanics and the effect on breathing pattern of high flow oxygen therapy in stable hypercapnic COPD. Thorax. 2017;72(4):373‑375. doi:10.1136/thoraxjnl‑2016‑209673
- 6. Luo JC, Lu MS, Zhao ZH, et al. Positive End‑Expiratory Pressure Effect of 3 High‑Flow Nasal Cannula Devices. Respir Care. 2017;62(7):888‑895. doi:10.4187/respcare.05337
- 7. Mauri T, Galazzi A, Binda F, et al. Impact of flow and temperature on patient comfort during respiratory support by high‑flow nasal cannula. Crit Care. 2018;22(1):120. Published 2018 May 9. doi:10.1186/s13054‑018‑2039‑4
- 8. O'Driscoll BR, Howard LS, Davison AG; British Thoracic Society. BTS guideline for emergency oxygen use in adult patients [published correction appears in Thorax. 2009 Jan;64(1):91]. Thorax. 2008;63 Suppl 6:vi1‑vi68. doi:10.1136/thx.2008.102947
- 9. Beasley R, Chien J, Douglas J, et al. Thoracic Society of Australia and New Zealand oxygen guidelines for acute oxygen use in adults: 'Swimming between the flags'. Respirology. 2015;20(8):1182‑1191. doi:10.1111/resp.12620