我们的智能 ICU 呼吸机。下一代


我们的智能 ICU 呼吸机。 下一代

在大屏幕上。 重要通气数据一目了然

嘘! 不要唤醒您的病人
平均噪声 35 dB,它是我们最安静的呼吸机。
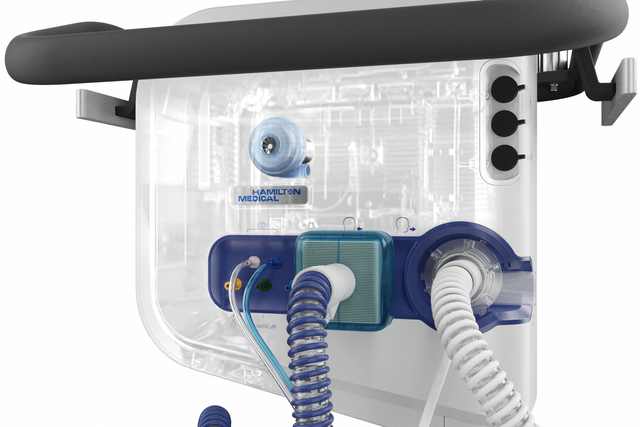
保证持久耐用。 我们的高性能涡轮
凭借强大的涡轮,此 ICU 呼吸机完全独立于高压空气出口和外部压缩机。这可最大程度提高灵活性,让您可以在医院里自由走动。 我们也在 HAMILTON‑C6 呼吸机的预期使用期限内对涡轮提供质量保证。

湿化器控件和状态。 呼吸机显示屏上
从呼吸机显示屏上舒适、直接地操作 HAMILTON‑H900 湿化器。 HAMILTON‑H900 与呼吸机同步,并根据通气模式自动选择湿化模式。

极度独立。 无压缩空气且由电池供电




设计与众不同。 选择适合您的需求的设置
这款呼吸机安装非常灵活!您可以将其装在台车上,连接到悬挂系统上,拆下其显示器或将其安装在台架上。
全局数据。 适用于 PDMS、监测和 EMS 的综合连接解决方案
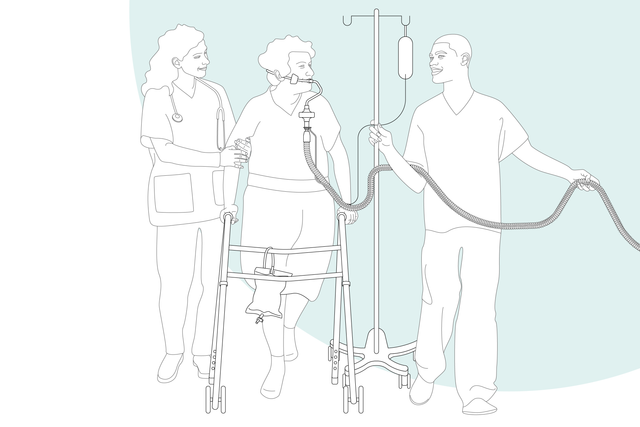
越快越好。 早期活动
凭借高性能涡轮、电池、紧凑设计和先进的通气模式,HAMILTON‑C6 还在病人旁边帮助病人期初下床活动。
想要查看更多信息?
探索 3D 模型
从各个角度了解 HAMILTON‑C6 ICU 呼吸机,点击热点,以了解更多信息。
快速了解详情
- 标配
- 选项
- 不可用
| 病人组 | 成人/儿童、新生儿 |
|---|---|
| 外形尺寸(宽x深x高) | 423 x 250 x 415 mm(监视器) 360 x 250 x 394 mm(呼吸机主机) 640 x 560 x 1400 mm(含台车) |
| 重量 | 监视器(交互面板)(不含固定架):7.8 kg(17.2 磅) 监视器(含固定架):10 kg(22 磅) 呼吸机主机(含固定架):10.5 kg(23.2 磅) 呼吸机主机、监视器和台车:46 kg(101 lb) |
| 监视器尺寸和分辨率 | 431.8 mm(17 英寸)对角线 1920 x 1200 像素 |
| 可拆卸式监视器 | |
| 电池运行时间 | 一块电池 1.5 小时 两块电池 3 小时 |
| 热插拔电池 | |
| 气源 | 集成涡轮,保修期为 HAMILTON‑C6 呼吸机的预期使用期限 |
| O2 接头 | DISS (CGA 1240) 或 NIST |
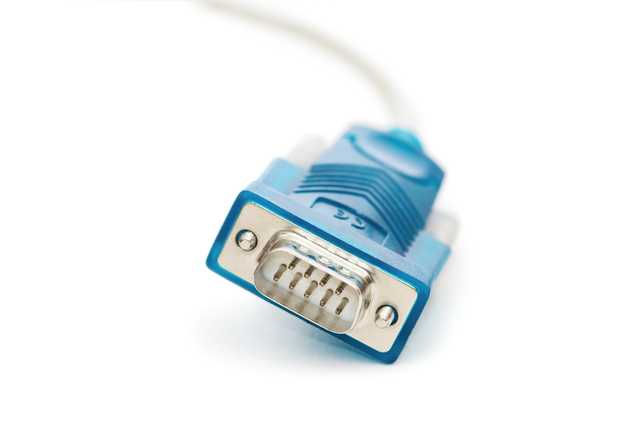
| 连接 | 3 个 COM 端口、2 个 USB 端口、DVI、护士呼叫器端口 |
| 音量 | 37 dB(在正常运行情况下) |
| 容量控制、流量控制 | |
|---|---|
| 定量、适应性压力控制 | |
| 智能通气 | ASV®、INTELLiVENT®‑ASV®(选项) |
| 无创通气 | |
| 高流量 | |
| 肺力学指标可视化(动态肺) | |
|---|---|
| 病人呼吸机依赖性可视化 | |
| 食道压测量 | |
| 二氧化碳图 | |
| 氧饱和度监测 |
| 肺复张性评估和肺复张 (P/V Tool Pro) | |
|---|---|
| 人机同步 (IntelliSync+) | |
| CPR 通气 | |
| Hamilton Connect 模块 |
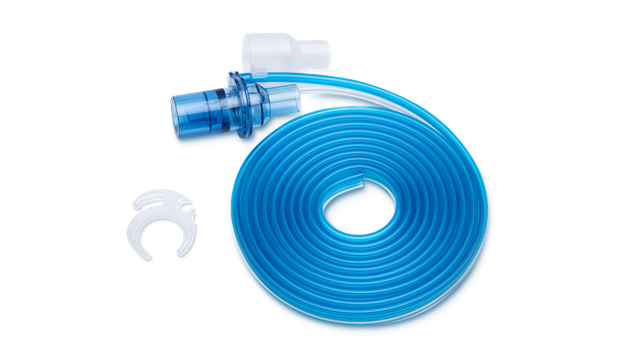
| 远程连接至 HAMILTON‑H900 湿化器 | |
|---|---|
| 集成 IntelliCuff 气囊压力控制器 | |
| 集成气动雾化器 | |
| 集成 Aerogen 雾化器 | |
| 与 Sedaconda ACD‑S 麻醉剂输送系统的兼容性 |

客户评语
One of the pearls of these ventilators is the interface. I think the interface of the HAMILTON‑C6 has a completely new level of monitoring capabilities.
Dr. João Alves
Intensivist, Internal Medicine and Emergency Department since 2018
University Hospital Center Lisbon, Lisbon, Portugal
用于您的病人
ASV® ‑ Adaptive Support Ventilation®。 适用于全天候适应
根据病人的肺力学指标和呼吸用力,ASV 通气模式每天 24 时从插管到拔管连续调整每次呼吸时的呼吸频率、潮气量和吸气时间。
INTELLiVENT®‑ASV。 适用于床旁辅助
INTELLiVENT‑ASV 智能通气模式持续调整病人的通气和氧合状态。
它根据临床医生设定的目标值和病人的生理输入设置分钟通气量、PEEP 和氧浓度。
IntelliSync®+。 适用于人机同步
IntelliSync+ 通过每秒数百次波形持续分析波形,能够立即检测病人用力和循环,并实时启动吸气和呼气。
IntelliSync+ 适用于有创和无创通气,无论采用哪种通气模式。
P/V Tool®。 适用于肺评估和复张
您可以使用 P/V Tool 评估肺复张性和确定肺复张策略。
此外,您也可将其用于进行持续充气肺复张操作和测量肺容量的增加。
跨肺压监测。 适用于内部见解
跨肺压监测可优化 PEEP、潮气量和吸气压力(
将其与 P/V Tool 配合使用可评估肺复张性和执行肺复张术。
远程湿化器访问。 便于使用
通过独特的呼吸机连接选项可以直接从呼吸机的显示屏上操作 HAMILTON‑H900 湿化器(
湿化器也可以根据所选的通气模式自动选择湿化模式(有创、无创或高流量)。
集成雾化器。 适用于额外治疗
集成气动雾化器完全与吸气和呼气时间同步。
集成同步 Aerogen 雾化系统作为一个选配件提供 (
输送药物气溶胶粒子的细水雾有助于您恢复支气管痉挛、提高通气效率和减少高碳酸血症 (
Integrated IntelliCuff®。 适用于控制气囊压力
IntelliCuff 可实时对用户设置的气管内插管或气管切开插管的气囊压力进行持续测量和自动维持 (
高流量鼻导管治疗。 适用于通气专家
高流量鼻导管治疗(
容积二氧化碳图。 适用于 CO2ntrol 狂热爱好者
近端流速和二氧化碳测量使我们的呼吸机能生成最新的容积二氧化碳图,为评估通气质量和新陈代谢活动提供生要依据。
呼吸机状态面板。 适用于准备撤机者
通气状态面板显示与病人的呼吸机依赖性相关的六个参数,包括氧合状态、CO2 清除状态和病人活动。
各栏中上下移动的浮动指示器显示给定参数的当前值。
快速撤机。 适用于独立思考者
快速撤机是 INTELLiVENT‑ASV 模式的一个功能,其可提供对病人状况的持续动态监测和控制,从而评估病人是否适于拔管。
自动 SBT。 适用于自主呼吸者
自动自主呼吸试验 (SBT) 是 INTELLiVENT‑ASV 模式中快速撤机功能的一部分,并为您提供执行全控型 SBT 的选项。
动态肺面板。 使用目视监测者
动态肺面板向您显示下列重要监测数据的实时图表视图:
- 顺应性和阻力
- 病人触发
- 氧饱和度
- 脉率
可配置的环图和趋势图。 适用于统计员
呼吸机可根据所选的监测参数组合显示动态环图。有了趋势图功能,您可以看到针对您选择的监测参数和时间框所显示的趋势数据。
设备持续将监测参数保存在其存储器中,即使在待机时也不停止。
脉搏血氧计。 适用于氧饱和度热衷者
氧饱和度选项提供集成无创氧饱和度测量,数据方便地显示在您的呼吸机上。
我们还提供氧饱和度传感器的全面组合方案。
高性能无创通气。 适用于面罩佩戴者
无创通气模式提供压力支持流速切换的自主呼吸(NIV 和 NIV‑ST 模式)和压力控制时间切换的指令呼吸 (NIV‑ST)。
与使用压缩空气的呼吸机相比,我们的涡轮驱动呼吸机能够提供更高的峰值流量。这就保证了即便漏气严重也具有最佳性能。
nCPAP 模式。 适用于小病人
nCPAP 模式的设计使您仅需设置期望的持续气道正压。之后,根据病人状况和潜在漏气调整流速。这就防止了意外峰值压力的产生,保证了高效的漏气补偿,并帮助减少了氧气消耗。由于压力测量灵敏度很高,流速的调整非常迅速。
为您提供

预组装。 且可直接使用
我们预组装的呼吸装置包括操作呼吸机所需的基本耗材,而且方便地放在一个包装袋中。
我们的所有基本耗材都专门为保证制造商质量的 Hamilton Medical 哈美顿医疗公司呼吸机开发。

减少人工操作。 更适应您的病人
为管理通气,您通常需要设置多个参数,例如,压力、容量、吸气和呼气触发、气囊压力等。每次您的病人状况改变时,您需要进行一次或多次调节。
为简化此过程和减少人工操作,我们创建了一系列解决方案:
适应性支持通气 (ASV) 是一种根据病人的肺力学指标和呼吸用力连续适应呼吸频率、潮气量和吸气时间的通气模式。研究表明,ASV 可缩短各种人群的机械通气时间,而且手动设置更少 (
IntelliSync+ 至少每秒一百次连续分析波形信号。这使 IntelliSync+ 可以立即检测病人用力情况,并实时启动吸气和呼气,因此替代传统的吸气和呼气触发设置。
气囊压力管理的常规解决方案需要您手动监测和调节气囊压力。
IntelliCuff 通过连续测量和自动维持所设置的成人、儿童和新生儿病人的气囊压力,安全管理病人的气道 (

帮助随手可得! 屏幕上关于故障排除的帮助内容
无论何时出现问题,呼吸机都会利用报警灯、声音和信息栏警示您。
屏幕上的帮助内容向您提供有关如何解决报警的建议。

撤离呼吸机! 实施撤机方案的工具
我们希望我们的呼吸机尽可能快速与病人脱离。因此我们向您提供工具帮助您实施您的撤机方案。
其中包括旨在鼓励自主呼吸的可视帮助和通气模式。

掌握窍门! 学习路径和教学内容
我们的在线学院提供易于遵循的学习路径,以使您尽快熟悉 Hamilton Medical 哈美顿医疗公司产品和技术。
面向未来
不断革新。 扩展您的呼吸机的能力
我们不断努力进一步革新我们的产品。添加新的功能和改善现有功能,以确保您在您的呼吸机寿命期间始终拥有最新的通气技术。


识一而知全部。 通用用户界面
无论用于 ICU、MRI 科室或病人转运,所有 Hamilton Medical 哈美顿医疗公司呼吸机的用户界面操作方式均相同。
我们的通气酷屏将复杂的数据集成到直观的可视化图像。
完整解决方案
完全集成的附件
我们围绕最高病人安全性和易用性开发我们的附件。我们尽可能将附件集成到我们的呼吸机,以简化整个呼吸机系统的操作。
我们的耗材

与我们的专家交流。 讨论您的需求
我们的通气极客团队很乐意帮助您选择最适合您临床护理环境的通气设备,并帮助您实现治疗目标。获取个性化报价或安排电话回访,了解更多信息。
有关更多信息
HAMILTON‑C6 the next generation of intelligent ICU ventilators ‑ brochure
HAMILTON‑C6 Technical specification for SW version 1.2.x
Hamilton Medical One solution, every situation
IntelliSync®+ brochure
Transport and storage solutions for the HAMILTON‑C6
参考文献
- 1. Kirakli C, Naz I, Ediboglu O, Tatar D, Budak A, Tellioglu E. A randomized controlled trial comparing the ventilation duration between adaptive support ventilation and pressure assist/control ventilation in medical patients in the ICU. Chest. 2015;147(6):1503‑1509. doi:10.1378/chest.14‑2599
- 2. Tam MK, Wong WT, Gomersall CD, et al. A randomized controlled trial of 2 protocols for weaning cardiac surgical patients receiving adaptive support ventilation. J Crit Care. 2016;33:163‑168. doi:10.1016/j.jcrc.2016.01.018
- 3. Zhu F, Gomersall CD, Ng SK, Underwood MJ, Lee A. A randomized controlled trial of adaptive support ventilation mode to wean patients after fast‑track cardiac valvular surgery. Anesthesiology. 2015;122(4):832‑840. doi:10.1097/ALN.0000000000000589
- 8. Chenelle CT, Oto J, Sulemanji D, Fisher DF, Kacmarek RM. Evaluation of an automated endotracheal tube cuff controller during simulated mechanical ventilation. Respir Care. 2015;60(2):183‑190. doi:10.4187/respcare.03387
- 100. Dhand R. New frontiers in aerosol delivery during mechanical ventilation. Respir Care. 2004;49(6):666‑677.
- 101. Waldrep JC, Dhand R. Advanced nebulizer designs employing vibrating mesh/aperture plate technologies for aerosol generation. Curr Drug Deliv. 2008;5(2):114‑119. doi:10.2174/156720108783954815
- 104. Baedorf Kassis E, Loring SH, Talmor D. Should we titrate peep based on end‑expiratory transpulmonary pressure?‑yes. Ann Transl Med. 2018;6(19):390. doi:10.21037/atm.2018.06.35
脚注
- a. 并非在所有市场均有提供
- b. 仅适用于 HAMILTON‑C6/G5/S1
- c. IntelliCuff 自动模式并非在所有市场均有提供
- e. HAMILTON‑H900 不适用于转运
- f. 也称为高流量氧疗。此术语可与高流量鼻导管治疗互换使用。